Conversations on Health Policy 2024: Year- end Reflections
As 2024 draws to a close, we take the opportunity to re-share the full series of “Conversations on Health Policy” published by the RTH Collective over the course of the year. We also take a moment to reflect on the series as a whole and on the intent and directions with which we undertook the building of this web resource and our hopes for its evolution.
Each of the nineteen conversations listed below addresses some of the major contemporary challenges related to health policies and health systems that come in the way of achieving the Right to Health and Healthcare. We say some rather than one because when it comes to health and healthcare no single, major challenge, no matter how well-defined and delineated is ever discrete. Therefore, we approach each of these challenges as a “problematic,” by which we mean a long-standing problem with many determinants admitting a variety of solutions based on context and the theoretical frameworks and ideologies brought to bear on it.
The dominant ideological stream within health-sector reform tends to view these problematics as inherent to public services. As a result, it follows that the solution lies in privatization or market-based reforms. However, three decades of experience with market-based reforms have shown that such reforms do not work out as theorised and in practice, in most situations, increase inequity. On the other hand, from the perspective of those who defend public services and believe that they should be provided as public goods, these problematics are seen primarily as symptoms of the lack of adequate public investment and accountability measures. From this, follow calls for greater investment, along with better enforcement and accountability within the existing design of public healthcare systems. Yet, over time, public health practitioners who have been struggling with addressing these problems within diverse organisational contexts and institutional fields of power, find that as crucial as public investment is, there is more to the problems involved; it is not simply a case of redoubling or reinforcing an older approach. In fact, the failure to address many of these challenges despite greater investment in public health, and the numerous difficulties in fixing accountability within public systems often ends up fuelling the main argument in favour of market-based reforms. And there we remain stuck.
It is here that the Conversations in Health Policy enters and hopefully offer a way forward. By engaging with persons who bring both deep and diverse experiential and academic knowledge, we try to approach these longstanding and complex challenges with renewed empirical and theoretical rigour and imagination and to discuss and deliberate in detail but with as much conceptual clarity as possible. In each case, we build on the important progress that has been made. For instance, the National Rural Health Mission (NRHM) did call for and attempt a number “architectural corrections,” and significant beginnings were made with reforms related to decentralisation, community engagement, professionalisation, and learning from innovation. Unfortunately, these efforts were largely incomplete and half-hearted. But perhaps even more important, while they generated a new positive momentum and effort, reforms struggled to sustain without an analytical framework for strengthening public health systems within which institutional re-design and change management could be fully understood, engaged and owned at all levels.
The Conversations, therefore, begin with a shared understanding among all of us in the collective that better, more contextually-engaged theorisation is not an academic exercise but is vital for meaningful public deliberation. For those within government and working in public systems, such frameworks—and an analysis of their underlying assumptions—are even more important and need to be widely discussed and debated. Unfortunately, though there are volumes of theory that support market-based reforms, there is much less contemporary theory that supports strengthening health systems as public goods, and even less that is publicly disseminated and discussed. One reason why such alternative theory is scarce is that most theoretical frameworks, emerge largely in western universities, and this relates to the political economy of how knowledge is generated, and gains approval and acceptance. When it comes to our own contexts, best practice and case studies are permissible, but not theoretical development.
The Conversations in Health Policy is a small but committed response to the paucity and possibility of attempting to better theorize these problems in ways which are more consistent with health equity and health rights and developed within and in response to our own diverse contexts and our own public systems, as they actually exist. In the process, we not only arrive at an explanation of why both market-based solutions and business-as-usual are not going to work, but we also offer grounded perspectives on the ways forward. Here, we attempt to re-think and work out a range of social, economic and political arrangements for health and healthcare for all, and in each case we pay attention to the technical and administrative aspects of healthcare and how they relate to each other. We understand health systems are complex adaptive systems and they have to be designed to be learning-adaptive systems to address these problematics.
Unsurprisingly, we have also adapted along the way! The first few “conversations” were constructed as essays, but that limited us to certain types of references and did not provide enough scope for sharing experience and for dialogue. Subsequently, we experimented with formats and became much more explicitly conversational, which we found helped us bring out the issues and complexities more clearly.
The nineteen Conversations include disease-specific programmes, health systems components, global health policy, national health programmes and the problems of measurement. Our metrics tell us that on an average we have a readership of about 5000, largely but not solely within the public health community, as very broadly defined. The feedback has been very positive and has encouraged us to keep at it. However, since many of those who follow these conversations began to access them later in the year and may not have been aware of the earlier conversations, we now circulate a list of all the conversations published so far. We hope this makes access to your topic of interest—and other related topics—much easier.
All these conversations are available on the website https://rthresources.in/.
The website also has a section on best practices and case studies that could be of interest to those in teaching health policy and systems studies. We look forward to expanding the collection over the next year. The website also has a growing collection of articles on important themes and sub-themes within the area of health policy and health systems studies. The thematic areas section aims to provide curated access to publications and reports relevant to each area. A number of these publications have been authored by members of the collective over their years of work within the system and from their contributions to civil society advocacy for health rights. This collection of papers is also very much a work-in- progress.
All this work is voluntary and done with limited resources. In some of these key issues, we hope we have managed to get a meaningful conversation going and provide fresh insights. We are also very encouraged by numerous follow up conversations we have had with policy decision makers, public health resource persons, and most importantly with students around these issues. Our aspiration for the coming year is even greater participation, with more contributions on a wider range of themes, more follow-up conversations, and deeper deliberations on health policy, accessible to all.
Wishing you a very happy and thoughtful 2025!
– From all members and friends of the RTH Resource Collective
Conversations 2024
There has been very limited comments on the media and even in academic journals on the major changes in the strategies of tuberculosis, globally and at the national level.
Preparations are on for the High Level Meeting of the United Nations on Antimicrobial Resistance, scheduled for September 2024. The proposed strategies are welcome but incomplete. There is much more that a Call for Action should address…
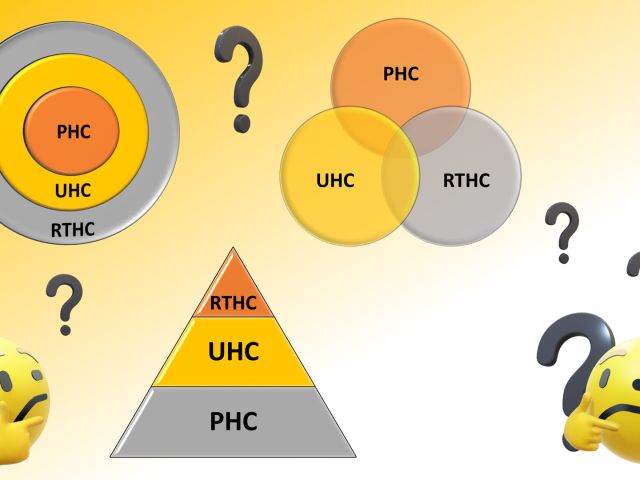
A better understanding of these three concepts and the relationship between them is essential for progress towards realization of the right to healthcare. One cannot be achieved without the other…
This is a picture of a 18 month old girl with severe pain due to dactylitis. Needless suffering. !!. The current policy is aspirational but flawed and needs to get it’s priorities right …
Much of what is said in the Negotiating Text of Pandemic Agreement is necessary and welcome. But is it sufficient to ensure that we never again have to experience the social, economic, health and human rights catastrophe that we have just been through during the Covid 19 pandemic??”
Four years after the pandemic, we have learnt a lot about it. But there is a lot we do not know as well. This is a time for reminding ourselves of what we went through and learning from it- so that we can truly say– never again !!
The challenge is to secure ASHAs own rights as a woman and a front line health worker, while continuing to strengthen her solidarity with the community as part of an alternative vision of an organization of health services.
We know that markets do not work to assure quality health care!! But what does? Over the last 15 years, the NHM has developed the National Quality Assurance System (NQAS) to assure quality in public health services. What is NQAS? Is it working? Is it scaleable? Is it enough? This conversation between Yogesh Jain and Sundararaman, the 8th in our series, explores the answers!!
Global Health Policies in an unequal world are more the resultant of political dynamics than of the public good. Introducing the WHO Tracker, a unique and powerful tool created by PHM, which empowers public health professionals, practitioners and policy makers in developing nations to understand and intervene in global policy setting and its adaptation to local needs. Use this to follow the ongoing discussions in the 77th World Health Assembly at Geneva.
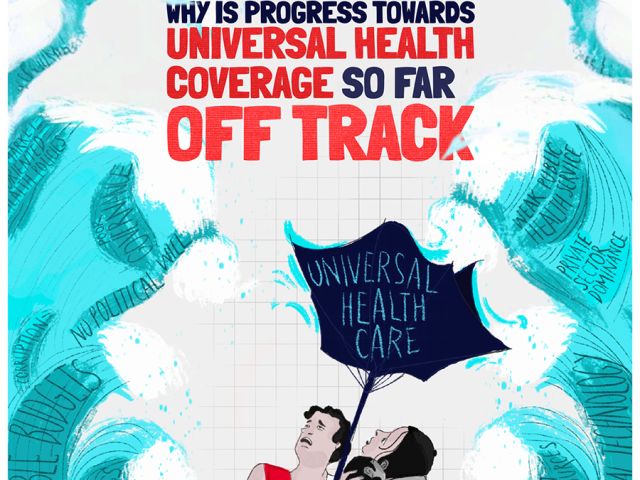
“Universal Health Coverage” was once hailed as “the single most important concept that public health has to offer.” ( Margaret Chan, 2012). But , even by WHO and UN assessments, it is off track, across most low and middle income countries !! In this conversation we look beyond implementation issues and disruption due the covid pandemic, to more basic questions about UHC as a strategy and as a discourse.”
India has the necessary digitized data systems in place to provide us with the mortality data we need, but yet due to some critical disconnects, we remain reliant on external global institutions for even state and national burden of disease estimates. In this conversation Dr. Chalapathi Rao, discusses how it is possible for state governments to generate reliable annual district level mortality information- even in the short run.
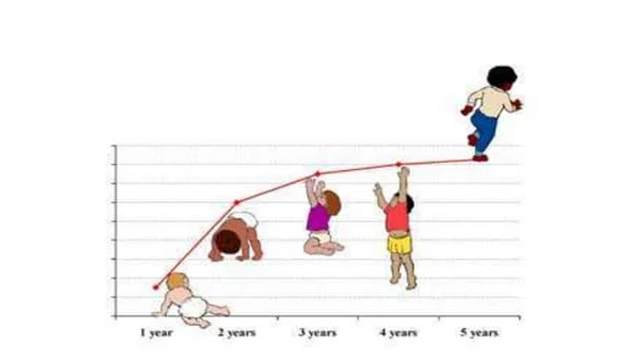
Last year, the ICMR initiated a process re-revisit WHO’s weight and height standards for children on grounds that these are not appropriate in the Indian context. But is this valid? Are current growth standards overstating India’s malnutrition crisis? In this conversation, Dr Yogesh Jain talks to Prof. Rakesh Lodha, AIIMS and Dr Pavitra Mohan,BHS, ( all of leading pediatric practitioners and academicians with experience in public policy) to clarify the issues and concerns underlying the current controversy and the values and goals that should inform our choice of standards.
The ESI is an amazing institution covering over 10% of the population. The ESI is conceptualized within a health rights framework and offers a basket of benefits that no other insurance programme even attempts. Yet when experts talk of UHC or publicly funded health insurance, the ESI is almost never mentioned. Performance in terms of delivery of benefits is poor, but this is not due to lack of funds, as the ESI has a huge surplus. This conversation is about how ESI must be saved, re-vitalized and expanded, as part of the struggle to achieve the right to healthcare and Health for All. And given some of the directions of reform that are being pushed, it it is also about how not to lose an asset that we never knew we had.
We are drawing attention to this recent publication from the regional WHO. In this introduction we highlight one context – the shift from selective to comprehensive care. We hope these case stories help the reader understand the complex nature of this shift, and provides grounds for optimism, that despite the challenges, such a change is feasible…..
The chronic shortfall of specialist skills in CHCs, cripples our ability to universalize comprehensive primary health care. Such skills are essential to provide referral support and continuity of care to primary care providers and patients. The persistence of the problem and the failure of many efforts to address this shortfall should lead us to introspect on basic design flaws. Drawing on national and international experience, we discuss how this gap can and must be addressed and that too on a priority basis…
A critical reading of the Progress Update is essential for those in engaged in practice or research in health systems and health policy. This conversation addresses some of the technical challenges of measurement, and implicitly its politics. What we measure as progress is closely related to where we want to go and how we intend to get there. To the average health manager and the health activist this could be heavy reading, but we hope that this conversation helps demystify health metrics, and make for more informed participation in “evidence-based decision making”.
The Ayushman-Bharat- Health and Wellness Scheme(AB-HWC), launched in 2018, is India’s big hope to deliver on the promise of universal and comprehensive primary health care- a logical extension of the efforts that the National Health Mission,2005 had begun. Its success would have paved the way for the realization of the right to healthcare. But in its rapid scaling up there has been weak conceptual clarity and many essential features of the scheme are under threat. Can the situation be retrieved? In this conversation, three public health practitioners who have been closely associated with its design and/or implementation discuss some of the urgent course corrections that the public health community could help with….
The ABDM is India’s ambitious push for digitization in the health sector. In this conversation, four researchers who have been associated with the design and implementation of healthcare IT systems, take a closer look at the ABDM and strive to understand what the program set out to do, what it has done and where it is headed. They explore what ABDM offers for the problems of access, equity and quality of care and the information needs of public health managers. Or has digitization become an end in itself? There are challenges but there are opportunities too….
Digitization of public health information systems has greatly increased the burden of data-work of frontline health care providers, reducing the time available for healthcare. But though huge volumes of data are generated, data-reliability remains low and its use in improving health outcomes uncertain. Ironically, HMIS, once the subject of health sector reforms, has now become one of its main objects. In this conversation, learning from the past, we propose some principles of design that would help develop HMISs that are more fit for purpose.
Private practice by government doctors is wide-spread, but far from universal. Further, even in places where it is allowed, the consequences due to the inevitable conflict of interests varies widely. Ongoing efforts towards mitigation also create differential impact. In this conversation we examine the justifications advanced and the principles that could guide public policy in this regard. We further discuss the various scenarios, and what we can learn from these different scenarios to chart our way forward.
Increasing reports of poor quality of medicines manufactured in India, whether as exports or for domestic consumption, are a matter of great concern. But this crisis should not become an excuse for strengthening corporate monopoly and excessive centralization. In this conversation, we discuss the why and how of designing a regulatory regime in India, that can guarantee quality medicines without any compromise to affordability or public health, not only for India, but for the entire third world.
Despite several recent policy initiatives, access to essential diagnostics remains inadequate across many facilities. As a result, patients continue to face out-of-pocket expenses : time delays and inappropriate care due to limited diagnostic availability in public facilities. In this conversation, we examine the barriers and the lessons learnt from existing models including the PPPs and explore strategies for improvement.
After arduous and prolonged negotiations, a global Pandemic Agreement has finally been adopted at the 78th World Health Assembly. But is this Agreement good enough to avert another pandemic catastrophe? In this conversation we invite Prof. Biswajit Dhar, to help us understand the public health implications of the Agreement in the context of the non-participation of the USA, the weaponisation of tariffs and a changing global economic order. And on what developing countries need to do further…
India’s incidence of breast cancer may be less than in developed countries, but its mortality is much more. In adult women of the 30 to 69 age group, this is now one of the top two or three causes of mortality. The introduction in 2017, of universal screening for breast cancer as part of public provision of comprehensive primary health care was a huge and highly welcome step forward. Eight years later, we take stock of where we have reached in implementing this policy and the challenges being faced, and why our understanding of primary health care needs to go far beyond what we offer as primary level health services.
Despite the many declarations of elimination, leprosy persists as a significant public health problem whose contribution to suffering and disability is seriously underestimated . In this conversation, three public health practitioners with decades of engagement with leprosy control at both field and policy levels and who are still engaged with its management on a day to day basis, reflect on why active transmission of the disease persists; why disabilities continue to emerge even after cure and on the options for the way forward —beyond the rhetoric of elimination.