The Right to Healthcare, Universal Health Coverage and Primary Health Care: The Necessary Relationship
T. Sundararaman and Mekhala Krishnamurthy
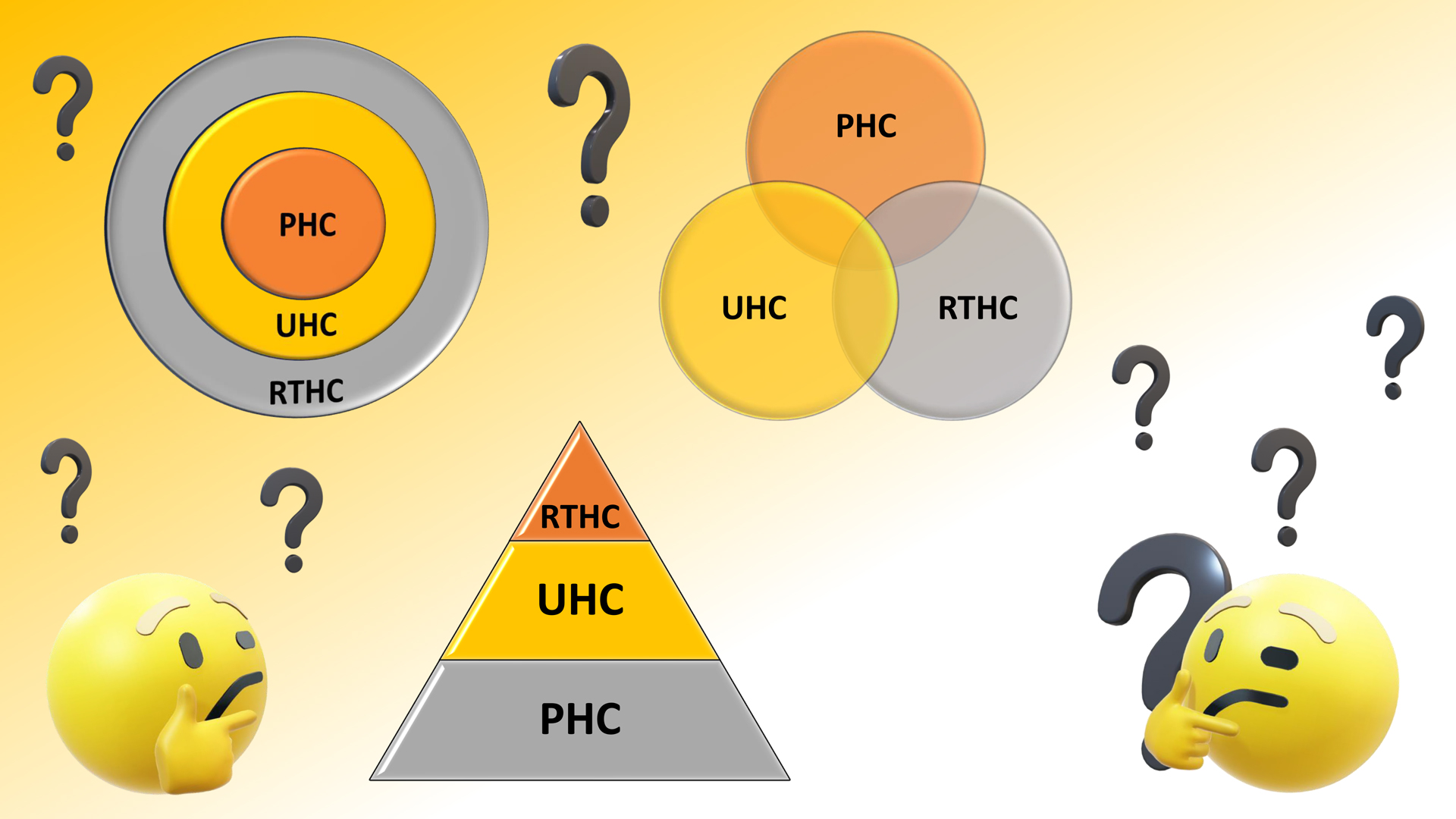
Three concepts – The Right to Healthcare, Universal Health Coverage (UHC) and Primary Health Care (PHC) – are all globally accepted as essential principles in the construction of health systems. It is important, however, to delineate how these concepts relate to each other and the variance with which the terms themselves are defined as well as the relationship among and between them as they come to be established in different strands of health policy discourse. This is important because the three terms are often either taken up as independent strategies (with various pathways) or placed in subordinate, linear, conflicting or contradictory relationships rather than first understanding each one clearly and then building up a relational perspective.
One approach to this task would be to take a semantic approach and to draw on published literature to map out all the variations and the alternatives they pose. Instead, the approach taken in this article is to engage with the debate as we have encountered it in the making of health policy in the Indian context and to bring in examples from other contexts, especially other Low-or Middle-Income Countries (LMIC) wherever appropriate to help inform the elements under contention today. In the process, the article attempts to establish the case for the necessary and essential relationship between these three terms in shaping and supporting the health systems we need to achieve the outcomes we seek.
Common Concerns with the Right to Healthcare
A leading administrator expressed the first problem posed by the legal Right to Healthcare in the following terms: “We are already doing all that we can do within our constrained resources for achieving UHC. What additional advantage would making it a legal right provide? It would only tie us down in litigations and contestations. Given both our constraints in human resource management and financial resources, we will hardly be able to close all the gaps. Further, this kind of litigation would then force us to change our priorities based on legal rulings.” Already in India, as senior administrators point out, court rulings on inclusion of costly treatments for rare diseases under public financing have created a challenge.
This is a tangible concern and has been expressed most in the Latin America context. A recent article in The Lancet put it this way: “the right to health provisions in national constitutions has led to the spectacular growth of litigation by citizens against governments where this right is enforceable in courts… In some instances, these cases have been brought forward by the rich, seeking high-priced medications and experimental treatments. In others, pharmaceutical companies have been found to have had an active role in bringing right to health cases to court. In countries such as Brazil, the right to health litigation has ultimately forced the state to foot the bill for costly drugs, such as onasemnogene abeparvovec, widely known as the most expensive drug in the world.” The article concludes with the caution that “We should be careful not to let loose language related to the right to health and UHC confuse or conflate these substantive and worthwhile goals” (Harris 2023).
This leads to the second major concern with right to health legislation: that the laws can be misused to serve corporate interests and agendas by enforcing public financing for expensive care with low cost-effectiveness and in so doing divert money away from the more essential care that remains widely required.
There is a third, somewhat looser argument that one frequently encounters. Perhaps it is more of a sentiment or symptom rather than an argument. One often hears that “a right-based approach has inherent limitations.” But, because this inherence is generally assumed and rarely illustrated, it is hard to contest and go against this drift. Yet, we caution against passively drifting into accepting this as received wisdom, without carefully questioning where this perception is rising from. One possibility is that there is a long and growing list of countries and state governments in India, that have legislated a right to health and healthcare but that this does not seem to make any difference in terms of outcomes. Assam is one case in point and many have already written off Rajasthan’s more recent law. There seems to be a pretty significant consensus here that the legislation does little to translate and sustain political commitment and institutional capacity and therefore leaves the unrealised right even weaker than the unlegislated demand. On the other, countries such as Sri Lanka were already doing a competent job of providing universal coverage before UHC policy arrived and without a right to health law. That they are now in danger of losing it due to financial and other crises is another matter and it remains unclear whether a legislation would have been able to prevent this. In India as well, states like Tamil Nadu and Kerala have been able to deliver better on healthcare coverage than most other states and they did so without enacting legislation. Either way you toss the coin, it can be argued that the right to healthcare doesn’t necessarily help and isn’t necessarily needed.
So, to sum up the arguments against bringing a law are: a) legislation is not enough to ensure delivery of health services as an entitlement; b) legislation leads to a burden of litigation and contestations that would not be productive in terms of increasing access in a resource-constrained setting c) legislation could be used to serve a corporate agenda forcing the state to pay for costly care, especially for the wealthy, diverting money from more essential health services for those in greater need.
Dangers, Definitions and Destinies
Each of the dangers outlined above are real. But they are not inevitable. A great depends on first getting the definitions right and then in how they are translated in law, health systems and financial arrangements.
First, the right to healthcare is a subset of the larger right to health. Neither assures us of being healthy, which is equally, if not more dependent on individual behaviours and genetic factors and circumstances beyond anyone’s control. The right to healthcare is therefore defined as an act that assures that everyone has access to a set of healthcare services which are timely, of good quality, can be accessed without financial hardship, provided with dignity, comfort of rights of the users and provided without discrimination (A more detailed description of right to health and health law is in general comment 14 of the ISECR, 2002) This implies that there is in place health systems that can deliver these services and that the government holds itself accountable for health provision. Thailand’s law expresses it even more simply: “Section 5: Every person shall enjoy the right to a standard and efficient health service as provided in this Act….The type and scope of health service entitled to a person shall be as prescribed by the Board” (NHSO Act, 2002).
A health system capable of delivering all healthcare services as needed would also be consistent with the official definition of universal health coverage (UHC). The definition runs as follows: “Universal health coverage (UHC) means that all people have access to the full range of quality health services they need, when and where they need them, without financial hardship. It covers the full continuum of essential health services, from health promotion to prevention, treatment, rehabilitation, and palliative care across the life course” (WHO). The right to healthcare and UHC therefore seem to definitionally and logically go together.
However, though in formal policy statements both the WHO and the World Bank take pains to emphasise that countries should be free to choose their own roadmaps to UHC, the experience over the last decade is different. In practice, unfortunately, UHC has become associated with a specific form of publicly-funded health insurance scheme that provides coverage for a limited set of services and for which financial protection, although formally assured, is seldom enforceable. This is why, especially in sections of civil society, the expansion of the acronym “UHC “as universal health care instead of universal health coverage is used to ensure that the term is meant to denote universal access and not to be trivialized to enrolment in an insurance scheme. What is even worse is that implicitly, but never overtly, the UHC discourse dismisses or ignores the task of strengthening public health services even though public services remain the most important source of health care with financial protection, especially for the poor. Since insurance is only a means of financing, in contexts where physical access to services is itself a problem, insurance has little to offer in terms of additional coverage. But perhaps the greatest limitation, and the one that places UHC at cross-purposes with the right to health, is the fact that one cannot enforce a right of access with an empanelled private provider. One could certainly make it a contractual obligation of the private provider to provide access as a right, but this is never fully enforced, and even the threat of enforcement leads to private provider exit. So as it stands, most eligible insured persons can be denied the benefits of the scheme by private providers and there is little recourse to preventing this.
There is an even bigger danger involved in the predominant model of publicly-financed private empanelled provision associated with UHC. Most publicly-funded insurance schemes work with a well-defined budget. The size of the budget is defined by the premium per family and multiplied by the number of families covered. This pays for a limited number of in-patient secondary or tertiary care episodes. For example a budget of about Rs 1200 crore may pay for about 800,000 claims. Now, if costly packages are introduced into the scheme, since it is profitable for private sector to provide these services or sell these medicines, the utilization of these packages would be higher, but it would displace a much larger number of necessary, and less costly services.
This displacement is not obvious. It often takes the form of insurance denial by third party administrators on procedural grounds. TPAs are tasked to keep the total approved claims within the budget limits. If budgets are allowed to expand then there is a shift of utilization to the costlier packages, which the more privileged are able to secure. Therefore, one finds that any right to healthcare which is linked to insurance schemes and where reimbursement is on a fee-per-service package basis and where the majority of providers are private providers is very likely a prescription for fiscal profligacy (or fiscal incontinence, as this has also been called) and health inequity.
Countries like Japan, Germany, Canada and Australia do have insurance schemes where the majority of healthcare providers are private providers. But, these are all health systems where all (or almost all) providers must be empanelled, all residents must be enrolled, all rates are fixed and applicable to all, and all working staff payments are also negotiated and fixed. Further, in countries like Japan, private profit from healthcare is specifically disallowed by law. To get to such a situation not only must a country be able to enforce such strict regulations, it must be also able to pay much higher fees to providers. Each of these countries have public health expenditure of at least 10 percent of GDP or more, and these are all high-income nations with very large GDPs. It is worth remembering perhaps that when Aneurin Bevan, the Secretary of State for Health and Social Care who set up UK’s National Health Services (NHS) under an Act of the same name was asked, how he managed to get all the private GPs on board, his response was “by stuffing their mouths with gold.”
These options are not available to any LMIC. In contrast we are looking at a model of UHC that works below 5 percent of GDP or even 3 percent of GDP. Or we can be politically incorrect and reframe the question: What is the level of universal health care that we can get and therefore the rights to healthcare that a health service can provide at a public health expenditure spend of 3 percent of the GDP?
Let’s take an example for us to think through. The costs of care for a cataract surgery of good quality even in the private sector is about Rs 8000 per eye, or about 16,000 for both eyes. The price of cataract surgery in the private sector would be anywhere from Rs 32,000 to Rs 100,000 for two eyes. But the maximum any publicly financed health insurance scheme is able to provide is about Rs 20,000 for two eyes. Hypothetically, we could get all private sector providers on board, if the minimum offer could be Rs 50,000 for two eyes, which we assume is the median cost, but that would mean that a lot of affordable care providers who now provide care at Rs 10,000 per eye (because they choose to opt for a high volume low mark-up business model or choose to serve low-income patients) would now also become high-cost providers of cataract services.
Clarifying Conditions and Key Design Features
Public Provision: It now becomes clear that any meaningful right to healthcare law in the context of Indian states is possible only if we have a system of universal health coverage in place, where the capacity of public health services and publicly administered services can cater to all those who need such services. The term publicly administered services is important here and refers to service providers who are privately owned but who choose to come under the ambit of health services as defined by the law through suitable contracts. It follows that any right to healthcare legislation must ensure that it implies the right to access a health service that can deliver healthcare responsive to the needs of the patient. The key design features of the health system through which such health services can be accessed as an entitlement must be indicated in the legal text.
Priority Setting: The next challenge is of priority setting. Given that resources are finite, how do we keep out those very expensive treatments and therapies that are of doubtful value and are clearly not cost-effective. Who is to decide and how is it to be decided what makes it in and out of the package and will such decisions stand in a court of law? The tried and tested solution is for the law to make it clear that the choices regarding the health services to be included as well as the costs of care that must be reimbursed to the providers would be defined by a duly constituted committee using a well-defined process. These committees need to be guided by both health technology assessment techniques centred around cost-effectiveness studies and a deliberative process that considers concerns related to equity and ethics. New procedures will have to demonstrate that they fall below an agreed cost-effectiveness threshold value and will have to prove that, given the available budget, the new services will not displace other essential care, which benefit many. It is well known that health systems like the UK’s National Health Services and Thailand’s Universal Coverage System have been using such an approach, and have developed institutions that have the capacity to make such assessments. This has been a protection against corporate capture and the courts have never overruled these decisions (at least as of date).
Non-confrontational forms of accountability: When it comes to avoiding any significant increase in legal contestations, putting in place a robust and fair grievance redressal strategy goes a long way. Thailand has what is called a no-fault liability clause in its act which ensures that errors and denials or illegal charges are compensated if found to be true, without necessarily having to fix which individual provider is to be held accountable for the same. This helps because often the gaps are systemic and medical errors do happen. One percent of the budget is earmarked for compensation and currently about 0.3 percent is spent. There is also a supportive local civil society arrangement that helps the complainant and ensures that there is a greater understanding among both providers and service users of the constraints, building solidarity instead of a confrontational form of accountability. But this requires the system to acknowledge errors and denials, which is after all the point of the law.
Thinking through the delivery mechanisms: The biggest problem that remains, however, is in ensuring effectiveness of a law in delivering healthcare as an entitlement. It is here that the necessity of a network of public primary health care facilities and providers becomes critical. This is not just any model-agnostic or experimental approach to UHC, but one that is consciously and foundationally based on a primary healthcare approach. The importance of the relationship between UHC and PHC cannot be overemphasized. Put simply: effective UHC requires a primary healthcare approach.
Understanding primary health care as an approach: A primary healthcare approach is a an approach to the delivery of services that is characterized by a few essential features. These could be listed as healthcare that is: comprehensive, prioritizes prevention and promotion, free, population-based, community based, people-centred and serves as the entry point to all levels of care. The characterization of comprehensive care must be contrasted against the earlier and erstwhile policy that called for selective packages, where only some aspects of reproductive health services and a few disease control programmes were included, with the rest being left to private markets. Even when some symptomatic relief for self-limiting illness was also included, this meant that over 85 percent of health care needs were not effectively covered. In the current understanding by contrast, most diseases have some aspects of care that are required to be delivered at the primary, secondary, and tertiary level.
The primary health centre provides services related to preventing these diseases and their early detection, and ensuring that even for chronic illness diagnosed at higher levels there is medication compliance and follow up and prevention of complications possible at the primary care level. Most importantly, when consultation at a higher level is required it is the primary care provider who acts as a guide and facilitator to access such care. Further, when we say this is community-based care we are referring to services being as close to communities as is convenient, which is what a network of primary level of care providers do. And when we say, this is population-based healthcare we are referring to the requirement that such a provider is responsible for the highest attainable health outcomes in the entire population and NOT ONLY to those who sought care.
Registration with primary care provider and entitlements: Thus, in such a health system, every family and individual is registered with a primary healthcare provider and such a registration is the means through which they access all preventive, promotive and curative services as required and feasible at that level. It is also the portal through which they have facilitated access to all the secondary and tertiary care that is available under the health service. In effect, the act of registration is the act of securing delivery of the entitlement. Patients who walk-in directly to a higher centre cannot be denied care, but they are not assured of the continuity of care across levels that they would get if they had come in as referrals from their primary facility of registration. In the current scenario, even where there are public services available, there are many informal forms of rationing care. Often patients are told to go elsewhere because the requisite care is not available there or because the available capacity is exceeded.
None of this is possible if UHC is equated only with insurance. It only works if there is a network of primary level care providers who are part of a UHC system designed on a primary health care approach. The delivery of healthcare services as an entitlement also requires a duty bearer, a site of prime accountability. A right to a public service requires a mandated architecture for delivery of that service where every individual knows where their entitlement lies and how it can be claimed. Such a law and system will be able to detect denials as a consequence of rationing of care and through mandatory referrals or expansion of services address this problem on a continuous basis.
Value addition at every stage of implementation and resource use: Such legislation will also enable the citizen or resident to claim their entitlement whenever necessary to call out denials to accountable authority structures. But perhaps most importantly, by clarifying where entitlements lie and the pathways to access them, a well-crafted right to health law that frames and protects a primary health care-based universal health coverage system would help guide health seeking behaviours so as to detect diseases early and get people to seek the most appropriate and affordable healthcare options in a timely fashion. Thus, at every level of resource availability and phase of the roll-out of UHC, a law brings greater clarity and appropriate utilisation. The Thai law puts it succinctly: “Section 6: Any person intending to exercise the right pursuant to Section 5 shall select a service unit for regular visitation, and shall be registered there as per rules and shall be entitled to the health services, as prescribed by the Board.”
The necessary relationship: We thus see that the right to healthcare requires universal healthcare which in turn needs a primary healthcare approach. The reverse logic is also true. To succeed, a primary healthcare approach needs a commitment to universal health coverage/care as defined earlier and achieving UHC requires to be protected by a law that ensures the nature of the service as a public good rather than as a market commodity.
This, then, is the necessary and essential relationship between the right to healthcare, UHC, and primary health care.
Necessary but not Sufficient:
Addressing the role and regulation of the private sector
One important question that remains to be addressed is that if delivery of the required health services is largely a public sector function, what then is the obligation on the private sector? Also, in a context like India, can the public sector provide health services as public goods if it is embedded within a large private sector? In the approach to the right to healthcare that has been discussed above, empanelment of the private provider within the health service delivery mechanisms of the act are optional and voluntary, never mandatory. But those who opt to participate can be facilitated. This is a system of all the services for all the people but is not inclusive of all the providers, in fact not even most of the providers. Under some circumstances, there can be some degree of mandatory contracting-in of private providers for public health emergencies and in some critical areas, but that is not the rule, it is the exception. Such an approach is also pragmatic, given the political influence of the private sector, and its own path of development.
With regards to the private sector there is of course a role for government intervention to set a level playing field for competition, by enforcing ethical and professional standards, preventing conflicts-of-interest and kick-backs, and by promoting transparency of rates, service availability and quality, and to some extent by regulating prices, at least when it comes to forms of price-gouging. Here, the government is acting on its commitment to protect health rights. Though such regulation is essential, these are better addressed under the Clinical Establishment Act and its rules which is distinct from the right to healthcare act.
Addressing social determinants
Another critical and troubling question also arises: what happens to addressing the social determinants of health? It is useful to conceptualize actions that address social determinants at three levels. First, is the set of preventive and promotive services that must be reached to families and local communities. These services are an essential part of a primary healthcare approach and therefore adequately covered under any right to healthcare law. The second set of interventions relate to inter-sectoral actions. Though the health system does have a role to play, most inter-sectoral action requires other laws. An omnibus right to health law that covers everything is not a good idea because the duty bearers are different and accountability would become very difficult to establish. A separate and equally important law that most states would require is a public health law that would come under the departments of public health, though usually implemented by local self-government bodies. In addition, there are environmental laws, right to food laws, right to social security, right to employment etc., that different departments need to frame and implement. The third are the larger structural determinants related to basic questions about the nature of economic growth and equality. Each have their importance, and it is not useful to confuse them or expect one act to address both the right to healthcare and the right to health that flows from its social, commercial, and structural determinants. However, to the extent that the most effective form of delivering health education is inter-personal communication and that individual level preventive and promotive services are critical to health and wellness, a primary healthcare approach is all the more essential and plays an important (albeit not comprehensive) role in addressing the social determinants of health.
T. Sundararaman and Mekhala Krishnamurthy
This article is posted at the website www.rthresouces.in. For more background resources on this issue you could visit Right to health and health care in the same website.


Liked the article. Will share with others. Will see if anyone will translate in tamil and other languages. Thanks