
The Struggle of Memory against Forgetting :
Some Critical Reflections on the 4th Anniversary of the Covid 19 Pandemic
- T. Sundararaman & Yogesh Jain
Introduction
The capriciousness of memory!!! It was only four years ago, yet it is difficult to recall the Covid 19 days. They seem so unreal. Did we really go through them? Such extreme isolation. The excessive loss of friends and family members. The fear for one’s life and fear for the lives of loved ones. Fear of the unknown and great uncertainty about everything. It seemed as though our lives had come to a standstill, and we wondered whether we would ever get back to the normal routine. But, looking back at it now, it appears as if we had only hit the pause button, and life is back on its usual track. However, leaving behind an exacerbation of several negative and social trends: more inequality, more poverty, more unemployment, and yes, poorer health status.
The WHO declared the spread of Covid 19 to be a pandemic on 11 March 2020. India declared a nation-wide lockdown beginning from 23 March 2024. Both deserve to be called anniversaries. And being a death anniversary for an event that led to an estimated 7 million deaths (at least), it is time for a sober reflection.
Throughout the pandemic, from 15 March 2020, when the first of the papers (1) were circulated online, people’s science movements and people’s health movements brought out a series of situation analysis papers and policy briefs (2) that provided civil society of an understanding of the tsunami that had overtaken it. These policy briefs, at its peak had over a 100 activists and public health experts, formally or informally, contributing to it. These briefs were widely read and influential even within the media and bureaucracy, where it provided an alternative source of information and thinking about the pandemic and the state response to it.
Part I is about the current situation, with regard to the pandemic and what it means to say that the pandemic has ended. Part II is about what we now know about the measures used to control pandemics due to respiratory viruses.
Part I is about the current situation, with regard to the pandemic and what it means to say that the pandemic has ended. Part II is about what we now know about the measures used to control pandemics due to respiratory viruses.This paper picks up that conversation from where we last left off. Have we learnt the lessons of the Covid 19 years? And even more critically, do we really have clarity on the lessons of the pandemic? Have we asked the right questions
Part - 1
The Current Covid 19 Epidemiological Situation:
In an interview published in the Scientific American on February 6th, 2024 Maria Van Kerkhove, (3) interim director of the WHO’s Department of Epidemic and Pandemic Preparedness and Prevention, discusses where we are now and the threat the disease still poses. This interview is a good summary of the main characteristics of the pandemic as it is today. Officially, the WHO has declared an end to the COVID public health emergency in May 2023. But WHO also reports that the virus continues to circulate world-wide and that there were more than 11,000 deaths within a one-month period in the first month of 2024, and over one million reported cases.(4) Reduced testing and reporting would contribute to the under-counting, and looking at data based on waste-water testing, the circulation is over 20 times the reported incidence.
So how is this the end of the pandemic? At what point did we declare it to be an endemic disease? It turns out that when it comes to ending a pandemic, it is finally the people, and not the epidemiologists,(5) who have the final say. Let us look at the first flu pandemic of 1918. The first flu pandemic is known for its three waves, but a historical analysis points out that there was a later fourth peak that cost almost as many lives as the catastrophic second wave. But the fourth wave did not lead to a return of all the restrictions that were there earlier. Moreover, there were later peaks that were never described as a pandemic. Similar is the scenario with the Covid 19 pandemic.
The epidemiological feature that characterizes the end point of a pandemic is the absence of major peaks in severe illness or death. The disease is then said to have become endemic. But in practice, many sources posit that it ends when people’s behaviour changes to the earlier lifestyle, irrespective of the official declaration. This reference (5) quotes John M. Barry, author of the definitive book on the 1918 pandemic “The Great Influenza: The Story of the Deadliest Pandemic in History, “as concluding that a pandemic ends “when people stop paying attention to it.”” If that is so, then India’s pandemic (and that in most low- and middle-income countries (LMICs), which began in March 2020, ended by the end of 2021, around 18 months after it started. Its first peak was in August-September of 2020 and a second peak in April-May of 2021, both of which did huge damage. India’s third wave of January 2022, in contrast, went almost unnoticed, with limited social restrictions.
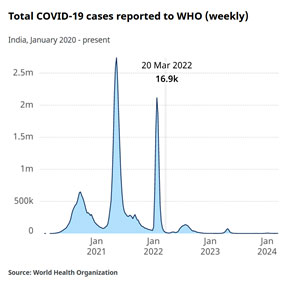

Source: WHO Covid 19 dashboard (6)
But what do we mean by stating that Covid 19 is now in the endemic phase? A simplistic understanding of disease incidence having reached some sort of flat-line graph is misleading. There will continue to be spikes and troughs and even plateaus, for the country as a whole and certainly in regions and sub-regions. A lot of our emphasis in the early writings on the covid pandemic was on the R0 number, and a value of R0 < 1 was associated with endemicity and R0 > 1 with epidemic spread. We find little mention of this in recent reporting, perhaps because this number can vary so much across regions.
The Evolving Virus:
What currently determines spread? It is a combination of the virus’s virulence, and the availability of vaccines and population level immunity. Mortality will relate to outcome to therapeutics for the very sick.
Epidemiologists and virologists monitoring the strains of the virus in circulation are forever looking out for strains which are more transmissible, that cause more severe disease and that has significant immune escape, which would mean that people would really need to get revaccinated right away. Surveillance categorises them into variants of interest (VOI) Variants under Monitoring (VUM)/ Variants of Concern (VOC).
Globally, SARS-CoV-2, JN.1 is currently the most reported variant of interest (VOI, now reported by 115 countries), and accounted for 90.3% of sequences. Its parent lineage, BA.2.86, has been declining and accounted for 2.2% of sequences. The overall evaluation is that these virus strains are of low additional public health risk at the global level. The WHO is currently tracking (7) five VOIs: XBB.1.5, XBB.1.16, EG.5, BA.2.86 and JN.1; and three variants under monitoring (VUMs): XBB, XBB.1.9.1 and XBB.2.3.
Evolutionary biologists who study evolution of these viruses inform (7) us that the trend is towards viruses becoming less severe, and spreading more rapidly at times, but with less injury. Many respiratory viruses like RSV have shown such a pattern. Seasonal flu also behaves similarly, although from time-to-time there are antigenic shifts that could lead to a dangerous epidemic affecting adults as well as children. Other influenza B type viruses do not change as much, and therefore they break out in children who have no past exposure to the virus.
Case Fatality Rates and transmissibility
Covid 19 has so far behaved like other respiratory viruses. Though the number of cases and deaths were far higher in the second wave, the disease was more severe and the risk of death was 1.49 times higher during the first wave. The overall CFR was 1.16 per 1000 person-days (PD), which declined from 1.80 per 1000 PD during the first wave to 0.77 per 1000 PD in the second wave. (8).However since the numbers of those infected were much higher, the number of deaths were also much higher in the second wave. The second wave was largely driven by the delta variant, known for higher transmissibility, but not for more severe disease (some studies did show a higher CFR, though!). The third wave was related to the Omicron variant, where the disease’s severity was even lesser, though to a large extent this was due to the protection vaccination that was offered. There are several reports of the disease having been more severe in the unvaccinated.
However, evolutionary biologists also caution that there is no such law that as evolution proceeds, virulence will decrease. In the worst-case scenario, it is quite possible that a virus strain may emerge, that is highly transmissible and has a higher case fatality rate and is capable of immune escape, viz. past infection or current vaccines do not provide adequate protection.
Part - II
What do we know about Pandemic Response Strategies? And not know about them!!
The virus is still here, it is still evolving, it is still causing deaths and we still do not know enough about its long-term effects. The question we ask now, as we reflect over the last four years’ experience, is what have we learnt that would help us prepare and deal better. Without doubt the Pandemic Agreement and the amendments to the International Health Regulations would be important legal and global instruments for a better response. The focus of these discussions is on technology-based counter-measures. But in this article, we take stock of some specific pandemic response strategies that were deployed during the recent pandemic and what we have learnt about them. These include:
- 1. Masking and Other Non-Pharmacological Methods
- 2. Lockdowns
- 3. Surveillance
- 4. Test, Trace and Treat
- 5. Vaccines and Vaccination
- 6. Long-Covid
1. Masking and Non-Pharmacological Methods:
Are measures like masking, hand hygiene and physical distancing effective? There are two questions here. Does an individual wearing masks have a lesser risk? Another, if this is used as a public health approach, does it interrupt transmission? Both have been controversial issues that have not been resolved adequately. What is the current consensus of expert opinion?
The authoritative Cochrane issue (9) on the effectiveness of masks in preventing transmission and reducing risk for respiratory viruses has this to say:
“There is uncertainty about the effects of face masks. The low to moderate certainty of evidence means our confidence in the effect estimate is limited, and that the true effect may be different from the observed estimate of the effect. The pooled results of RCTs did not show a clear reduction in respiratory viral infection with the use of medical/surgical masks. There were no clear differences between the use of medical/surgical masks compared with N95/P2 respirators in healthcare workers when used in routine care to reduce respiratory viral infection. Hand hygiene is likely to modestly reduce the burden of respiratory illness, and although this effect was also present when ILI and laboratory-confirmed influenza were analysed separately, it was not found to be a significant difference for the latter two outcomes. Harms associated with physical interventions were under-investigated. There is a need for large, well-designed RCTs addressing the effectiveness of many of these interventions in multiple settings and populations, as well as the impact of adherence on effectiveness, especially in those most at risk of ARIs.”
But the jury is still out on the issue. The authors themselves caution that their results may reflect the practical issue of many persons in the studies not following the masking guidelines rather than an absolute failure. But then, the Cochrane review is based on studies from 78 RCTs which include use of masks in both laboratories confirmed influenza and Covid 19 pandemics.
There are many individual studies that assert a beneficial effect. One cluster randomized trial in Bangladesh on community level interventions to support masking and physical distancing compared both outputs and outcomes with control villages. The study showed a tripling of mask use in intervention villages to reach a coverage of 42% of the population and this led to a 9.5 reduction in sero-positive cases and 11% reduction in symptomatic cases. Physical and social distancing changed much more modestly. The duration to which the change in behaviour lasted is also reported in the study. (10). There are official reviews like the one by The Royal Society (11)which affirm that all measures used were indeed effective. But these conclusions seem to be based entirely on observational data from some of the best-case country examples within the high-income countries.
One big controversy at the global level was regarding the difference between droplet transmission, which was the early focus of preventive measures and aerosol transmission, that later gained emphasis, with the WHO being blamed for not having given the latter sufficient emphasis. Droplet transmission is caused when coughing or sneezing by an infected person leads to droplets of saliva being projected and falling within a space of about one metre. Susceptible person is at a risk of acquiring conjunctival or mucosal infection by infective droplets or through contact with fomites on surfaces. In contrast, in an aerosol the droplet is less than 5 μm in diameter, and it can be dispersed wider and stay in the air longer. The current opinion is that both routes of transmission occur and the aerosol route implies that the virus stays viable and infective in the air in closed or poorly ventilated rooms for a longer time. There is also little controversy that a person who has illness is less likely to disseminate it as extensively if wearing a mask . Taken together a strong recommendation made for avoiding meetings in enclosed spaces and wearing masks if such a meeting is inevitable, remains valid.
However, the considerable hype and stigma and inflexibility associated with the advice on masking and the physical distancing methods needs to be re-visited. There are many situations like when driving on roads, where masking has little role, but was nevertheless insisted upon and enforced by security agencies, mainly because they could do so. Or like subjecting individuals to spraying by disinfectants. In particular, given what we now know between the balance of benefits and risks, one needs to be much more cautious about imposing such guidelines on all populations at all times. It is well recognized that people living on the margins had greater difficulty in observing these restrictions and yet they bore the brunt of the enforcement measures. But there is very little that was done then, or has been studied since on how to address social and economic inequity and the balance of power, when insisting on individual compliance.
It is well recognized that people living on the margins had greater difficulty in observing these restrictions and yet they bore the brunt of the enforcement measures. But there is very little that was done then, or has been studied since on how to address social and economic inequity and the balance of power, when insisting on individual compliance.
2. Lockdowns:
Pandemics have occurred many times in the past and quarantines have been imposed. But such lock-downs are unprecedented. Even the term is new to public health, and cannot be found in any standard text-book. Lockdowns are often discussed as part of non-pharmacological interventions which is partly true but largely misleading. In a quarantine those who are suspected of having been infected are kept in isolation till the disease manifests itself. It could mean the population of a particular city if the disease is known to have spread widely there. But in a lock-down, it is the healthy population who are being quarantined from being exposed to an unknown source of disease as a form of interruption of transmission. In India, it was expressed as preventing community transmission from setting in. If that was indeed the goal, it miserably failed. If the objective was to give time for counter-measures to become pandemic-ready, or of reducing cases from peaking and preventing overwhelming of hospitals, then there could be a case for a judicious, evidence-based application of some social restrictions.
We now know a lot about the adverse impacts of the lockdowns. There are now a significant body of publications on lockdowns. Several studies that have documented the adverse impact of lockdowns on food security, on livelihoods, on the economy, on education, on mental health and on gender relations (12). Most of these studies have also pointed out huge increases in inequity on every economic and social parameter. Not only journal publications, but there are many books as well. One example of such documentation are the case studies from India, Angola, Argentina, Ghana presented in the book Pandemic Response and the Cost of Lockdowns (13) . In particular Kunal Purohit’s chapter “How the World’s Harshes Lockdown Unleashed a Humanitarian Crisis” documents how it led to the largest and most rapid human migration seen in India since the Partition. Another detailed source material on the impact of the lockdown on the poor is the book- Covi 19, a view from the margins, edited by Yogesh and Sarah (14).
There are a number of studies and papers on the loss of lives due to disruptions in different health programmes, and this includes tuberculosis and HIV control, care in pregnancy, child immunization, non-communicable diseases, cancers and mental health. What we do not know with the same degree of certainty is whether the lockdowns helped reduce the spread of the virus and the morbidity and mortality associated with it, and whether these benefits outweighed the hardships and loss of lives the pandemic-induced lockdown caused.
But would that balance of benefits and risks apply to population groups across countries and within countries where the vaccines never reached, or reached far too late and too inadequately? Were the lockdowns worth it? We have almost no publications in this area.
The Royal Society study, examining this question for high income countries, concludes that “The effective application of NPIs ‘buys time’ to allow the development, evaluation and manufacturing of such therapies and vaccines at scale. So, there is every reason to think that the application of combinations of NPIs will be important in future pandemics, particularly at early stages with novel pathogens when there are knowledge gaps and when therapeutics and vaccines are not yet available.” Fair enough. But what about other populations like in Africa where there were stringent lockdowns, but the vaccines never reached.
A related question is about the stringency and proportionality of lockdowns and the ways used to enforce the lockdowns. A lockdown could be a universal stay at home order (or curfew) where only certain essential services were permitted, and even this was defined narrowly. It could mean closure of public transport, or of all transport including personal vehicles. It could mean shutting down of markets. It could mean closure of work-places and of schools and other educational institutions. The stay at home could be 24 hours long, or it could take the form of night curfews or weekend curfews. The boundary of the shut-down could be a block of apartments or a street, or a concentric circle of a few kilometres around a known disease incidence, or the whole town, or district, or province or country. Many of these decisions were taken by the security apparatus of the government with little reference to the public health community. But has this been subject to public health review since?
Those who agreed with more stringent lockdowns were generally those with good social security, and living conditions and where work-from-home possibility existed. For them the precautionary principle was everything. An example “We do not want to send our children to school since we are afraid they would get covid. We know that covid has no serious adverse effect in most children, but we have to be cautious since it may have a long-term effect. And even if it is only one or two children why take the risk.” Or the argument may go “we know that covid 19 does not spread much in an open environment. The probability of catching the virus from someone going past in a scooter or walking past you on the road is very low. But it is possible. So why not insist on mandatory enforced masking even in such circumstances.”
But for those with no social security, or who need to go to work daily, or where living conditions are poor, it is proportionality that is the main issue. Is the suffering and risks that a specific population faces due to restrictions outweigh those faced due to the disease? Would not the principle of Common but Differentiated Responsibilities and Respective Capacities, which has been applied to medical counter-measures, equally apply to the issue of social restrictions?
The reality is that we really do not know the answers to any of these questions, and there is little ongoing research or expert committees at work trying to answer them either. The chances are that if we have another pandemic, we may experience the same madness all over again, with little learnings even in finetuning decisions and processes of social restrictions better than we did before. Several chapters in the book (13), “Pandemic Response and the Cost of Lockdowns”, looks at some of the determinants of this silence.. It has some chapters that reflect on why such an enquiry did not take place. One of these is the way the boundary of what could be debated got drawn within the policy community and in the public discourse, with some considerations a priori being labelled as inconsistent with a scientific outlook. In high income countries, right-wing politics, made an uneasy alliance with science sceptics and industry interests to deny the seriousness of the pandemic and this made democratic discussion on these issues within the scientific community difficult, with sceptics of the lockdown having to subscribe to the group-think on the issue. Second, was the systematic ignoring of proportionality and equity concerns, in favour of an overly precautionary approach. And third, was the difficulty of challenging any opinion which was considered as “rooted in science” as identified by whoever were declared the authority figures within science. One author (of the chapter on proportionality of response) concludes: “To be fair, the respective ideas whose far-reaching absence in the public discourse I bemoan in this chapter- thinking more about the costs of lockdowns to freedom, questioning the relevance of average age of the people dying of covid 19, questioning the preference given to the protection of life over other considerations- were all at one point considered and discussed. But they were rejected too quickly and eradicated from the realm of respectability too fiercely, leaving the lockdown endorsing strategy as the only acceptable one and pushing the discussion of alternatives into the public sphere.” (page no 167)(13).
The reality is that we really do not know the answers to any of these questions, and there is little ongoing research or expert committees at work trying to answer them either. The chances are that if we have another pandemic, we may experience the same madness all over again.
There is clearly a need for a democratic and scientific discussion on lockdowns, and this needs to be informed by evidence, as much from the humanities and social sciences as by virologists, immunologists and clinical science. Public health as an integrative discipline, straddling both the biomedical and the social science could take a lead role in this. But there is an even more important role for public health expert in this discussion. Paraphrasing Virchow, public health experts are or ought to be the natural attorneys of the poor (Virchow referred to it as physicians). Considerations of equity in the causes, consequences and responses to the pandemic needs to be factored in with much greater clarity in the response to future pandemics. The extensive violations of human rights across countries due to coercive enforcement of multiple social restrictions and mandates must not be seen as sporadic implementation failures, but reflective of a deeper malaise in which the public health and policy community share responsibility. The entire discussions of the Pandemic Agreement and the amendments to the IHR misses these aspects almost completely.

3. Surveillance:
A lot of effort in the pandemic treaty goes into the getting a commitment on surveillance and early reporting. High income countries would like to know as soon as possible, preferably within 24 hours of any outbreak of concern. But what do we need and how near are we in meeting our objectives? And if the disease surveillance system of a country is not robust enough to meet its requirements, can it ever generate reliable information for cross-border and international use?
When the Covid 19 pandemic hit our shores, India already had in place a fairly robust surveillance system for flu like illness and severe acute respiratory illness under the National Centre for Disease Control (NCDC). Quite inexplicably this reporting ceased and instead a parallel chain of reporting where general administrators collected data of only confirmed covid positive cases without any links to presumptive and symptomatic cases took over as the main system. For most of the pandemic, the NCDC was not active. There was a more aspirational Integrated Health Information Portal (IHIP) being rolled out at that time under the NCDC, which also hit the pause button in deference to the covid 19 specific reports. After the pandemic peaked, work on IHIP resumed, but it still did not reach the performance levels required of it. Something similar happened to the registration of deaths and different forms of death reporting. Though routine death reporting was very incomplete in some of the central and northern states, it had reached fairly high levels of completion and reliability in the better performing states of the South, West and North. The medical certification of cause of death was centred around medical college data and not fit for the purpose, but with some increase in frequency and periodicity of reporting, this could have aided disease surveillance greatly. Instead what happened was that even the usual cause of death reporting slowed and the Sample Registration Survey, which has reported on time for the last few decades, has not yet reported for 2021. Based on the death reports that some states had published, international estimates of excess mortality during the pandemic were released that showed much higher mortality than the government estimates. The Government has contested these reports, but till now it has not published its own data-sets.
A stand-alone system of reporting individuals testing positive for covid 19 from each center as the basis of monitoring the pandemic is not fit for the purpose of even the pandemic, let alone for normal times. What is required is a health systems approach and not a stand-alone surveillance mechanism.
A stand-alone system of reporting individuals testing positive for covid 19 from each center as the basis of monitoring the pandemic is not fit for the purpose of even the pandemic, let alone for normal times. Unless test positive cases are corelated with cases with suggestive symptoms and with deaths and with other causes of similar symptoms, little reliable knowledge to guide action will be generated. The learnings therefore can be summarized as follows:
- The FLI/SARI surveillance and reporting system should be strengthened as part of the Integrated Disease Surveillance Programme, and this must remain the basis of surveillance even in the eventuality of a covid resurgence.
- The current IHIP portal and protocols are problematic. There is a need to review these to ensure that only essential data which is within the capacity of facilities to generate as part of their regular work is collected. ad, that the system is geared to decentralized analysis and prompt district level esponse to this information on flow.
- Good quality disease surveillance with completion of reporting requires that there is in place a network of primary care providers whose services are utilized by a majority of those with healthcare needs and that they have the laboratory and specialist support for diagnosis; not only suspected covid cases, but all acute illness that could be part of the differential diagnosis.
- There are a number of ongoing efforts to strengthen routine death reporting so that over 90 percent of deaths are reported with a presumptive cause. Such data should be anonymized, aggregated and available at district and state level, every few months, or at least annually and subject to review. This data is already on flow and for the most part computerised- and so this is more a problem of willingness rather than technical capacity or infrastructure.
In summary- what is required is a health systems approach and not a stand-alone surveillance mechanism. It is likely that public health opinion in the National Centre for Disease Control would be aligned to these suggestions. But such are the high stakes and powerplay around information, that one anticipates that achieving these four rather obvious standards above will be rather challenging.
4. Test, Trace and Treat:
The rapid scaling up of testing for covid 19 using the RT-PCR tests was undoubtedly one of the great achievements of the Covid 19 response. From less than a dozen tests a day to a few million tests in 9 months was a huge achievement. It involved being able to develop the test, scale up production, improve access to an increased number of diagnostic centres and manage the logistics and supply chain management that was required to go with it. However all of this depended critically on being able to access the pathogen and its genome in time. Manufacturers also need to access enough samples of all variants of concern so as to be sure that their tests are valid. But so far that has not been a problem.
It is not surprising therefore that access to the pathogen has become the key point of negotiation in the pandemic agreement, and it’s a make-or-break issue. Access to pathogen is required for tests and for vaccines and for therapies and Big Pharma can make billions of dollars in profits if they get this access without an obligation to share the benefits. Most of the testing is likely to remain based on public expenditure, and that would mean an assured market even in low income nations. There is also hopeful news or even newer and simpler tests being developed.
What is the statement with regard to therapeutics? Hospitalization for moderate or severe disease identified by reduced oxygen saturation remains the norm. For moderate or severe disease where there is low oxygen saturation or hypoxia, short duration steroids have a proven role. But steroids have no role in mild cases to prevent onset of de-oxygenation. In moderate and severe cases heparinization with low molecular weight heparin is recommended. In severe progressive disease, not responding to the above remdesivir and tocilizumab have a limited role. While supportive hospital care makes a significant difference to mortality, there are no specific antivirals that prevent the development of severe disease that are widely in use.
At the international level nirmatrelvir-ritonavir combination has a strong recommendation as a first line drug preventing progression to severe disease. Other drugs are still being tested. For severe disease a combination of steroids, IL-6 receptor blockers and Biricitinib has been recommended. There are few reviews on the extent of use of these.
What is important to note is that most of the widespread modern medicine therapeutics that were extensively used during the pandemic, by both public and private providers, have not been approved. All of these were introduced despite lack of the WHO or any serious expert body recommending it. There is now enough evidence to state that these drugs have no role. The most recent protocol for treatment of covid 19 in India specifically cautions against use of any of the following a) Lopinavir-ritonavir b) Hydroxychloroquine c) Ivermectin d) Neutralizing monoclonal antibody e) Convalescent plasma f) Molnupiravir g) Favipiravir h) Azithromycin i) Doxycycline and the use of steroids in mild cases to prevent progression. So while on one hand there was a lack of access to appropriate care, there was a virtual explosion of inappropriate care. In their introduction to the book Covid 19, A View from the Margins, Yogesh Jain records that due to unregulated and inappropriate over-prescription of steroids, India saw over 40,000 cases of devastating fungal infection- mucormycosis. Whereas most other countries which had even greater covid prevalence and access to treatment hardly saw any. (14)
But we need to reflect on how many of these drugs were widely recommended by public and private providers and even by sections of civil society, despite the lack of evidence or even evidence of ineffectiveness. While it is easy (and to these authors, appropriate) to dismiss efforts at homeopathy or traditional medicines as unscientific solutions, the support for some of these came from those “rooted in science.” Clearly there was a lack of trust on expert opinion, both because of weak understanding of how science and scientific evidence. works. One must also remember the psychological aspect – faced with fear, stigma, uncertainty, and a sense of powerlessness – people guided by those family members or physicians whom they trusted, made their choices on preventive and treatment protocols. In conditions of scientific uncertainty and ambiguity (when different experts voice contrary opinions), and fear, the levels of trust and transparency required are far higher, and there is a need to put protocols or standards in place to achieve this. (15)
Contact tracing is another long story. An over-reliance on digital solution which turned out a dud and an under-emphasis on community engagement and high levels of stigma all combined to reduce the effectiveness of this tool. Perhaps a regular familiarity with how contact tracing needs to be organized and needs to be built up within the primary health workforce as part of emergency preparedness. There have been very few reports on stigma as a determining factor and the determinants, (16). Consequences and inequities related to stigma is another area where more research inputs would be welcome.
5. Vaccines:
Information on covid vaccines is now widely available, and so are many discussions on this. However, for want of space we limit this article to just flagging key issues. One area where public information is much required is a comparative assessment of the wide variety of vaccines already available and those on the pipeline. We also note that there is considerable ambiguity on need for a booster dose of the vaccine, and if so which vaccine. At the policy level, there is also the larger question of what role did vaccines play in ending the pandemic. Pandemics came to an end across most nations at about the same time, irrespective of their achievement in vaccination. But the consensus is that universal vaccination saved lives, and failure to achieve this was costly. Another major issue was the need to make access to vaccination a universal entitlement, but be very selective on vaccine mandates. Low-income countries, which had the greatest challenges in ensuring universal vaccination were also most hit by vaccine mandates. This same contradiction existed within nations also.
Pandemics came to an end across most nations at about the same time, irrespective of their achievement in vaccination. But the consensus is that universal vaccination saved lives, and failure to achieve this was costly.
The issue of innovation, manufacture and access for the future dominates discussions at the global stage. One recent development was that closure on Dec 31, 2023, of COVAX, the multilateral mechanism established to accelerate the development and manufacture of Covid 19 vaccines and support equitable access to vaccines. This mechanism had been launched in 2020 by the Coalition for Epidemic Preparedness Innovations (CEPI), GAVI, the Vaccine Alliance, UNICEF, and WHO. In an article in Lancet (17) , marking the closure, the achievements of COVAX are described as “delivered almost 2 billion doses of COVID-19 vaccines and safe injection devices and nearly US $2 billion to support vaccination campaigns…. enabled by agreements with 190 economies across all income levels, making it one of the largest multilateral partnerships in modern history.” It further states “To maximise support to countries, the mechanism provided end-to-end assistance across research and development (R&D), manufacturing, policy development, regulatory systems, supply and country readiness assessments, transportation and logistics, storage, and administration, as well as monitoring and evaluation.” This narrative would be contested by most in low- and middle-income countries as the negotiations at the Pandemic Agreement show. It does not do justice to the tremendous challenges developing countries faced in getting timely access to vaccines they needed, even when excessive stocks were crossing expiry dates in high income countries.
Most independent commentaries on COVAX are far more critical. In one important comment on this issue David Legge writes (18) : “In March global cooperation around diagnostics, medicines and vaccines moved from WHO to the ‘Access to COVID-19 Tools Accelerator’, a new ‘multi-stakeholder public private partnership. The “vaccine arm” of the Accelerator was the Covax Facility which would mobilise donor funds to pay for vaccines for the 20% priority populations in low and lower middle income countries. By July however, it was clear that massive bilateral advanced purchase agreements by the high income countries would reserve most of the early supply of effective vaccines and jeopardise the fund-raising for Covax. The rise of ‘vaccine nationalism’ looks set to cause long delays in access to vaccination in many L&MICs, and significant morbidity and mortality as a consequence.” (2021). The paper recommends that solutions lie in full public funding of Covax and expansion of local production of vaccines supported by technology transfer and an immediate waiver of key provisions of the TRIPS Agreement. This was the narrative that was supported not only by wide sections of civil society, but also by most L&MICs. And this is one of the frontiers of contestation between high income nations and L&MICs in the ongoing negotiations on the Pandemic Agreement.
Long-Covid:
While Covid 19 is an acute infection that lasts less than 2 weeks, about 10% of those infected go on to develop long term consequences, purportedly due to persistence of the virus, or some form of abnormal immune response besides exaggerated blood clotting mechanisms. While the largest proportion of hospitalization was needed for lung related diseases, long-covid has a more protean and diverse organ involvement: involving blood, muscles, nerves, brain and other organs. Due to the inadequate understanding about its duration and pattern of involvement, over-attribution as well as denial of symptoms have been observed. It is not uncommon for many people to attribute almost any illness to its origin from their own acute covid illness. Yet over 200 symptoms varying from very mild fatigue to debilitating complications have been associated. Some serious ones include chronic fatigue, thrombotic and other cardiovascular disease, onset of diabetes, many cognitive symptoms, postural tachycardia, menstrual problems and a host of others are feared to persist for several years, if not long. Several such impacted individuals are unable to return to work causing impact on livelihood.
The diagnostic tests for many of these long-covid illness patterns are still under development, which hampers true disease burden ascertainment. While drugs to reduce inflammation and regulate immunity as well as few antivirals have been shown in specific long-covid illness patterns, there is a parallel set of me-too and drugs with unproven efficacy flooding the therapeutic space.
There is clearly a need to understand the pattern of long-covid illnesses as well as their causes. Further, we need to invest in the diagnostics and clinical trials on therapeutics for specific long-covid patterns. Presently, there is a lacuna in our response.
Has community vaccination reduced the risk of long-covid? Most studies do point towards some protection against long-covid, but the final word is not out yet.
In Conclusion:
The Covid19 pandemic is technically over, but it continues as one of the most important public health concerns of the day. There is uncertainty about its epidemiological course, but the scientific community has built enough tools and mechanisms to track these changes. There has also been great progress in the development of tests and vaccines. The major challenges in ensuring universal access to technologies for medical counter-measures are far from solved and as the current stalemate at Pandemic Agreement shows, may not be solved anytime soon, but at least the world is cognisant and seized with the issues.
However, when it comes to the science-society and the health systems interface, in almost all areas there is ambiguity as well as silence about both the lessons of the pandemic and where we go from here. The determinants of this could be many. One important aspect relates to the multiple challenges in making equity more central to the societal response. But perhaps, equally important, the entire covid period was a very traumatic experience to us all, individually and collectively. It was characterised by a sense of helplessness in face of overwhelming external events which we are loathe to recall – there is in fact a denial of what we did ( or could not do), and how we survived those days.
It is therefore important to remind ourselves of Milan Kundera’s profound statement- “ The struggle of man against power is the struggle of memory against forgetting.” Towards that end, we need to re-visit these questions and delve further into them.
Acknowledgements
Gratefully acknowledge inputs from Dr. Bitty Raghavan, Senior Resident , PSM Department, JIPMER- Karaikal, and copyedits from Dr. M.D. Sruthi,
References
- Sundararaman T. Understanding the COVID -19 epidemic and the demands of the Peoples Science Movements and Peoples Health Movements- Background Paper to the provisional Charter of Demands by Jan Swasthya Abhiyan (JSA) and All India People’s Science Network (AIPSN) 15 March, 2020
- Repository of AIPSN-JSA statements on the Covid 19 pandemic during pandemic times: (from 15 Match 2020 to 22 march 2022) https://resources.aipsn.net/node/45
- Meghan Bartels Rampant COVID Poses New Challenges in the Fifth Year of the Pandemic
- WHO COVID-19 Epidemiological Update, Edition 165 published 15 March 2024 https://www.who.int/publications/m/item/covid-19-epidemiological-update-15-march-2024
- Tanya Lewis, People, Not Science, Decide When a Pandemic Is Over, https://www.scientificamerican.com/article/people-not-science-decide-when-a-pandemic-is-over1/
- WHO Covid 19 Dashboard: https://data.who.int/dashboards/covid19/cases?m49=356&n=c
- Ewen Callaway December 9, 2021: COVID Variants Hint at How the Virus Will Evolve
- Bogam P, Joshi A, Nagarkar S, Jain D, Gupte N, Shashidhara LS, Monteiro JM, Mave V. Burden of COVID-19 and case fatality rate in Pune, India: an analysis of the first and second wave of the pandemic. IJID Reg. 2022 Mar;2:74-81. doi: 10.1016/j.ijregi.2021.12.006. Epub 2021 Dec 18. PMID: 35721428; PMCID: PMC8690685.
- Jefferson T, Dooley L, Ferroni E, Al-Ansary LA, van Driel ML, Bawazeer GA, Jones MA, Hoffmann TC, Clark J, Beller EM, Glasziou PP, Conly JM. Physical interventions to interrupt or reduce the spread of respiratory viruses. Cochrane Database of SystematicReviews 2023, Issue 1. Art. No.: CD006207. DOI: 10.1002/14651858.CD006207.pub6.
- Abaluck et al., Science 375, eabi9069 (2022). DOI: 10.1126/science.abi9069
- COVID-19: examining the effectiveness of non-pharmaceutical interventions –Executive summary Issued: August 2023, Royal Society DES8417_2
- COVID-19 pandemic: A review of the global lockdownand its far-reaching effects Helen Onyeaka1, Christian K Anumudu1, Zainab TAl-Sharify1,2, Esther Egele-Godswill3 and Paul Mbaegbu, Science Progress 2021, Vol. 104(2) 1–18
- Kai Moller, The proportionality of lockdowns and Anthony Mckeown in Lockdown Consensus and the Dangers of Performative Scientism” in Eds Peter Sutoris et al Pandemic response and the Cost of Lockdowns- Routledge Press, 2023,
- Yogesh Jain & Sarah Nabia Eds, Introduction in Book : Covid-19 A View from the Margins, Manohar Publishers, 2022,
- Françoise et al. Evidence based policy making during times of uncertainty through the lens of future policy makers: four recommendations to harmonise and guide health policy making in the future: Archives of Public Health (2022) 80:140 https://doi.org/10.1186/s13690-022-00898-z
- S Krithi, Kalpana Karunakaran, J Jeyalydia, R Parthesarathy, T Sundararaman.: Discourses around Stigma and Denial in the COVID-19 Pandemic A Case Study from Tamil Nadu EPW Economic & Political Weekly January 22, 2022 vol 57 no 4, pg 34-39
- Tomothy Jesudasan, Covax officially closes thelancet.com/infection Vol 24 April 2024
- David Legge, Sun Kim; Equitable Access to COVID-19 Vaccines: JOURNAL FOR PEACE AND NUCLEAR DISARMAMENT 2021, VOL. 4, NO. S1, 73–134 https://doi.org/10.1080/25751654.2021.1906591
Note : This article is posted at the website www.rthresouces.in. For more background resources on this issue you could visit conversation Health Policy in the same website.


This thought-provoking article, by Dr Sundararaman and Dr Yogesh Jain, reflecting on the fourth anniversary of the Covid-19 pandemic is timely and prompts deep introspection. This ongoing global crisis has not only reshaped our world but also challenged our collective actions as people, civil societies, health systems, and countries in the face of adversity. As we navigate this ongoing global crisis, your critical reflections serve as a reminder of the lessons learned during the Covid-19 years. And even more critically, have we learned any lessons from the pandemic? Have we asked the right questions? Have we agreed upon the answers? Have these answers shaped our current and future actions? And finally, how do we build a more resilient and compassionate future? Truly, your contribution to this discourse is invaluable.
This is such an informative and well-written post! I learned a lot from reading it and will definitely be implementing some of these tips in my own life