Why is Progress towards Universal Health Coverage so far off track? Implementation Failure or Gaps in the Strategy?
Professor T Sundararaman (TS) & Dr Shalini Singh (SS)

This conversation examines the current challenges of Universal Health Coverage (UHC), as pointed out in recent global meetings like the 77th World Health Assembly (WHA77) and the United Nations General Assembly’s High- Level Meeting on UHC(UNGA). It starts with exploring the global consensus that progress on UHC is lacking due to limited and inequitable funding, low political accountability, and human resource issues. However, it also examines the Peoples Health Movements’ view that this slow progress in addition to above factors also stems from flawed and incomplete strategies, not just implementation challenges. The discussion elaborates on Peoples Health Movements’ (PHM’s) insights and recommendations, addressing issues like lack of comprehensive indicators to track progress, issues with strategic purchasing, regulatory challenges and public sector service delivery weaknesses. It also discusses the validity of UHC as a goal, its missed opportunities and suggests potential areas for improvement
SS: We know that a lot of recent global reports have been stating that progress towards UHC is stagnating or worsening, especially between 2015 and 2021. So with regards to that, I just want to understand your thoughts and your perspective on why the world seems off track with regards to attaining this UHC agenda. And what are the urgent measures required at country and global level to address the problems?
TS: Before we start, would you like to define what you mean by universal health coverage? This term has been used in different ways in different contexts and perhaps we should level off on which definition of universal health coverage we have chosen to go with for this conversation.
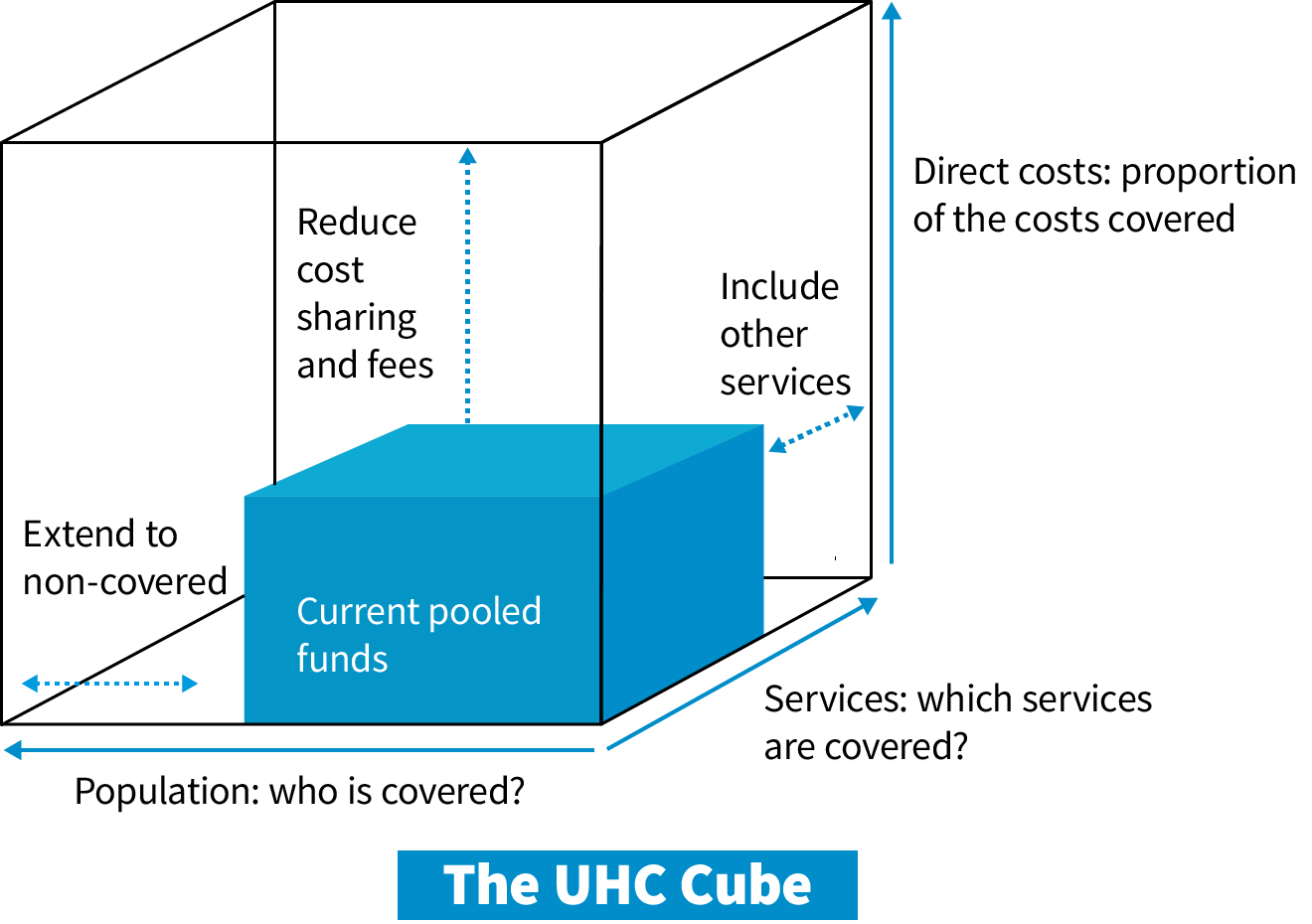
SS: I am going by the WHO definition: “Universal health coverage (UHC) means that all people have access to the full range of quality health services they need, when and where they need them, without financial hardship. It covers the full continuum of essential health services, from health promotion to prevention, treatment, rehabilitation and palliative care.” That is from the WHO website. We need to note that this is about healthcare services, and does not include the social determinants of health.
TS: And again, before I go into your questions, would you specify a bit more about what you mean by saying they are ‘off track’? What source are you going by and is it applicable to India also?
SS: Most of my understanding about UHC being off track is coming from this Global Monitoring Report of 2023. This has been cited in the Political Declaration adopted at the UNGA meet and in the report to WHA 77. These documents state :
“Trends in financial protection are worsening, with the incidence of catastrophic out of-pocket spending on health having increased from 12.6 per cent in 2015 to 13.5 per cent in 2019 and 4.4 per cent of the global population in 2019 were pushed or further pushed into extreme poverty due to out-of-pocket payments for health;” (para 18 b , Political Declaration of UN High Level Meeting on UHC, Sept, 2023).
As financial protection was the prime reason for adopting UHC, this is indeed a huge set-back.
The report also acknowledgse poor coverage in these words:
| “There is a global shortfall of 523 million people in achieving the commitment made in the political declaration of 2019 to progressively provide 1 billion additional people by 2023 with quality essential health services and quality, safe, effective, affordable and essential medicines, vaccines, diagnostics and health technologies; (Source: ibid, para 18 c)” |
As per the UHC service coverage index, the world moved from 44 percent coverage to 68 percent in 2015- and at that level it slowed down and since 2019 it has stagnated. Further much of this increase comes from Hugh Income Countries (HICs) and not from Low- and Middle-Income Countries (LMICs).
TS : First of all, we need to be cautious about using the UHC service coverage index. Most of its indicators relate only to a very selective package of RCH and the TB, HIV and Malaria control programmes; Two indicators for NCDs are added on, three indicators on health care infrastructure- but even with this,’ is a poor representation of coverage. These indicators could miss over 60- 80% of healthcare needs. There are better ways of measuring coverage. Another issue about these indicators that we need to ask is : whether it is enough to just measure service coverage, or should we also track progress in health outcomes like “preventable mortality” to better gauge progress on UHC? But before we go into this, I have one more question for you. Could you recall what the WHO itself says as the determinants of why it is off track?
SS: In the report presented in WHA77 four problems are identified. These are need for more funding, need to ensure the equitable use of that funding, need to strengthen the health and care workforce and orienting systems towards a primary health care approach. But I note that the Peoples Health Movement has taken a position which is very different from the rest of the civil society group, where you are saying that it’s not so much of an implementation challenge, but it’s a design flaw. What exactly are we indicating?
TS: Yes. I think all the 4 problems that WHO identifies are important and I think they provide a lot of the explanation. However, I am going to contest this as an incomplete explanation on the grounds that this lack of progress is not something limited to some countries. Surely every country can’t get it wrong. If the majority of countries struggle to fulfil the UHC promise, we need to move beyond implementation challenges—such as insufficient financing and workforce—to examine design issues and the broader structural factors influencing the situation. It’s crucial to assess whether the program has effectively addressed the underlying reasons for the UHC failure. In a systems analysis it helps to study a system as delivering exactly what it is designed to deliver. And if it is consistently not able to provide financial coverage and not able to provide the increased service coverage, then we must look at why this is happening as a common phenomenon across all LMICs. There is really no separation of implementation and policy failure. A policy is only as good as it is implemented. So that is basically the broad view with which we have proceeded, with a systems analysis to understand this.
We note that Covid pandemic did create a major disruption in progress. But since progress towards UHC was off track even earlier and continues to be a problem despite the attention that the health sector got due to the pandemic, we need to examine the strategies themselves.
SS: So what do you think are the problems with the current UHC strategy?
TS: Let me highlight three major main problems.
The first is the introduction of a policy discourse that calls for shifting of government role from provision of care to purchasing of care. The two main vehicles of purchase are publicly funded health insurance and public private partnerships. Country after country in LMICs have gone into these schemes. In many documents, the progress in UHC is measured by not the degree of public service delivery, but by the introduction of schemes where governments purchase care independent of who the providers are. Now that strategy has not worked. Publicly funded health insurances programmes fail to reach even the limited objective of financial protection and public private partnerships have seldom sustained. There is adequate evidence available to support this perspective.
The second is the huge parallel actively promoted growth of the private sector. WHO is silent on increasing presence and domination of corporate health care, the entry of venture capital, the billions of dollars of profits being made, and the growing political power of the corporate private sector. In fact, many global financial institutions are funding and promoting corporate private sector. Now, there is a facile assumption, that as long as we only look and strengthen what we do with public finances, what is happening in private markets won’t influence public health goals. The truth is that there is no Chinese wall between the two and therefore what is happening in the unregulated private sector has, through multiple pathways, has a direct influence on the overall status of financial protection and service coverage.
And the third is in solutions offered to strengthen public health service delivery itself, and the inadequacies of WHO guidance in this area. The WHO is seized of many issues related to health workforce management and the primary health care focus but has not been able to promote this in country circles. Another big issue is the lack of integration of vertical programs, most of it are vertical all the way into the WHO divisions. Then there are the problems of access to technologies, especially innovation and supply chain of newer technologies- including medicines, point of care diagnostics, medical devices etc. And the need to put a right to healthcare framework in place. The WHO mandate includes this last aspect and it’s reflected in its UHC indicators, yet the UHC discourse overlooks it. These are significant reasons for our inability to progress. Without these four crucial elements in public service delivery design—primary healthcare focus, integration of vertical programs, decentralized capacity with access to essential technologies, and a legal framework for healthcare rights—progress towards improved service delivery with financial protection will continue to lag. Adding to this are the two aspects the WHO emphasizes: the scarcity of human and financial resources, painting a clearer picture. So one gets a better picture on UHC when all these aspects are considered together.
SS: If there are few examples of success why is there a lot of focus and impetus in all the countries on the publicly funded insurance schemes? Why have most countries been driven towards dedicating public financing to support health insurance programs?
TS: The answer lies in the power of the policy/public discourse. In the new public health management discourse that became popular in the 1980s, that legitimized and justified privatization. public services are seen as inherently inefficient and of poor quality because market forces do not act on them. In health sector, the central problem was posed as people being forced to choose between poor quality public services and an unaffordable or expensive private sector. And the case is made that if governments opt for demand-side financing, it would let people choose where they want to go, public or private, and government reimburses whoever they opt for. The government acts as a purchaser. By giving choice to people, you are assuring both quality and efficiency which a public sector without competition and choice cannot provide.
Now when this was rolled out, the first observation was that the private sector was not willing to work at the package costs that governments were providing. Governments argued that they are providing a marginal cost and for marginal capacity, which is what is done internationally and that should be adequate to set a level playing field. (Marginal costs are the costs incurred by the hospital for seeing one additional patient, assuming that much of the investments are in place). However private sector sought higher price packages, based on opportunity cost. Many even estimated their loss on the basis of the prices they forego, and prices set in the market are much above even opportunity cost of care. In fact, the private sector cost of care is cheaper than the public sector because other than the specialists they pay every health worker less. With much higher reimbursement rates being sought or effectively taken through co-payments in breach of terms of the contract, the argument of efficiency goes out of the window. And in the very next stage, quality also does. Before choice and competition were to ensure quality. Now the whole private sector is saying that to provide quality care in the private sector, you need to incentivize quality with even higher rates of reimbursement. And then the sad reality is that even after this is conceded, private hospitals neither consider insurance enrolment as an entitlement to care, nor pass on the benefits of financial protection. The net result is that PFHIs relationship with private sector becomes a form of stimulus and subsidy to private healthcare expansion. In underserved areas, many specialists shift from the public to the private sector since insurance support makes this viable.. Once established, they can leave subsidized provisions, returning to unregulated market prices and weakening the private sector. Once they are established and private sector weakened they can exit the insurance empanelment and go back to unregulated market prices. The danger is, that unless special efforts are taken, we would have a weakening of the public sector, but not expanding the care provision.
Another problem with PFHIs , at least as we experience it in India, is that because budgets are limited, this insurance is able to cover only the inpatients care and that too for select procedures. All primary care is left out. All ambulatory outpatient secondary and tertiary care is left out. And within inpatient procedures, supply side factors make sure that the private provider chooses to place only a few packages on offer and there is no way of enforcing that the providers offer all packages to everybody. Even if that is the contractual terms. So not surprisingly, PFHIs makes no dent on out-of-pocket expenditures or on catastrophic health expenditure experience. On the contrary one acquires new problems in the form of moral hazards, or excessive and wasteful consumption of care. This could lead to utilization of care increasing, even while unmet needs remain the same or improve.
Similar problems exist in contracting for primary care. Public private partnerships is no longer a new idea. It is at least 25 years old. And after extensive work, except for some niche examples, the best we can say the is that some of the contracting has been able to provide good services on par with the public sector. Hence, the concept of purchasing to ensure efficiency, quality, or financial protection falls short in addressing this issue.
This is not a problem of just India or a few countries. PHM country circles who have been looking at this problem report similar issues with PFHIs in all their countries. Most studies in India show that the extent of OOPE experienced by an uninsured person in the public facility is still higher than what is the best level of financial protection provided to an insured person in the private sector. So it is public provisioning that acts as the greater vehicle of financial protection rather than purchasing mechanisms. Its only the strong influence of ideology as reflected in the policy discourse that keeps this going.
SS: Since publicly financed health insurance programs have been so uniformly adopted across nations, do you think there is some role of technical agencies here? Is the technical support which is coming for UHC across these nations somewhere contributing to this issue?
TS: I think so. In terms of a formal position global institutions insist that each country can have its own road-map and they are not insisting on any. However most major technical agencies set up for UHC are a part of this discourse where there is little support for creative strengthening of public provisioning of services and most of the effort goes into promoting forms of purchasing care. Take for example the Joint Learning Network for UHC sponsored by BMGF, World Bank and GIZ (German aid). Or Access Health International, and so on. This is not to question their sincerity. This is the way systems work. Aidagencies of select high income countries wfund much of technical assistance. And agencies with international presence access such funds and sustain work in health sector reform. . Their whole ideology allows them to believe that making public systems work means making it more market-like viz. introducing market like incentives and mechanisms and behaviours is what makes it work. So, innovation is almost equated with different forms of bringing market pricing and purchasing into the public sector. This trend is even more pronounced with Global Corporate commercial consultancies like McKinsey and Bains consulting and PricewaterhouseCoopers etc. Their main income is from consultancies to corporate houses and their own vision and experience is also largely corporate oriented. For an alternative form of development of public services as public goods, neither is there theory, nor is the scale of technical assistance large enough or good enough. A little bit happens in the WHO space. But that’s about it ,and WHO is not the major player when it comes to technical assistance. So if a country does decide to strengthen public health services as public goods, there is neither theory nor enough technical assistance support available other than that for disease control programs.
SS: Now moving on to the growing presence of a commercial and corporate private sector, how do we understand the challenges these pose and how can we address this?
TS: A recent news report (Sunday Express, June 2nd) states that “the health care sector in India has been witnessing record investments and in the past 5 months of this year, the industry has secured private equity and venture investment capital of $1 billion. The industry saw investments of over $ 4.5 billion across 19 deals in 2023, a 220% rise from last year. In 2022, the sector attracted $1.4 billion dollars across 15 deals.” The story goes on to relate that that hospitals have also expanded or announced their expansion plans. This is the scale. Also note that venture capital among all forms of capital accumulation demands the highest rate of return on investment. The company comes in with an investment, and exits after 5 to 10 years with something like 5 to 10 times the sum it has invested- a 500% return on investment. So corporate hospitals are seen as a very high growth industry.
These hospital serve less than 3-5% of the population, but in India, this is a large number. The issue is that their huge investments attract specialists and equipment, setting excessive standards in diagnostics and procedures nd distort market prices. Their monopoly on certain high-tech services and their high charges drives up prices across the private sector their charges become reference point.
This is not the scenario in most high-income countries with the exception of the US. In many countries like Japan, there are restrictions on profits and dividends in healthcare. In many countries it is a single payer system with both healthcare rates and worker salaries benchmarked across the country. Almost nobody can operate outside the insurance mode and insurance negotiations ensure that prices are kept within finite limits. Regulations are strict and well enforced.
So the sort of pressure venture capital is putting on hospital care in developing world cannot happen in the Japanese or European economies. But most emerging economies, including India are a soft target for global capital, hungry for super-profits. In India the healthcare industry grows at about 15% compared to about 7 percent for services sector and about 5 % for the economy as a whole.. Major financial firms are now entering in hospital and healthcare across all LMICs.
The consequences to health policy is that it becomes subordinate to industrial policy and the needs of having higher and higher economic growth rates. The incentives are for the government not to regulate. The corporate leaders also have an undue advantage in terms of public health uninformed influence over decision making in health sector. The public sector is remains to be constrained in areas of health care provision where the private sector flourishes but is required to take over responsibility where the private sector does not want to go. Like tuberculosis, whatever you try, private sector participation is weak and the blame of this is attributed to public sector. Whereas in high return areas like IVF (in-vitro fertility) or cancer and cardiovascular surgery the private sector dominates and public sector capacity remains under-developed. It would be important to put all of health care, including most of tertiary care as a public goods and have firm regulations on the entire private care industry.
There is also the huge problems created by the increasing privatization and commercialization of all health professional education. The high costs of such education make it unaffordable to candidates from more marginalized communities and under-serviced areas. Further with the burden of re-paying educational loans and debts, many cannot opt for public service. But most damaging is that these commercialized institutions impart values and an ethics that is not compatible with the development of healthcare as a public good.
The big gap that I’m seeing in the global UHC strategy is the failure to even point this out. Nowhere do global advocates of UHC consider the barriers imposed by the privatization of health professional education. Nowhere in the discourse are we acknowledging that the rise of corporate venture capital and huge investor firms entering into the hospital industry in a massive way is distorting the market. Can there be meaningful financial protection in a venture capital funded hospital? This is not part of the discourse. And this silence on the role of global capital and the financialization of the hospital industry is, I think, a serious flaw in the design.
SS: Agreed. Correct me if I’m wrong, but a large part of this push is deliberate, and meant to draw attention to the health sector as an investment opportunity. And this particularly becomes pertinent in nations like ours which have a very well-defined target of becoming a 5 trillion economy. So basically, you keep pushing all the sectors to contribute to the economic growth. It’s possible that such a paradigm is also supporting the phenomenon.
TS: Yes, these concessions to the commercial hospital industry is best explained by the fact that the economic policy increasingly sees hospital care as part of industrial promotion and investment policy and part of what drives the economic growth rates. Take for example the removal of all curbs on foreign direct investment in healthcare industry. This is consistent with the perception of private health sector as a high- growth area, driving economic growth, but not as a measure of financial protection. This priority would also be consistent with the finance ministry’s reluctance to increase invest in public systems that can potentially compete with the corporate provision of healthcare and prevent it from monopoly pricing. In this discourse, public health care and welfare becomes equated with “freebies”. In liberal democracies, whether they are welfare states, or social democracies, public expenditure healthcare is seen as an investment, albeit a long term investment. Almost all high income countries have understood and done this. Even in low income countries, Costa Rica and Thailand are doing much better in economic growth because of their investment in health care. However, on an average finance secretary and policymakers responsible for financing just do not understand this concept. They would be comfortable in investing in mega infrastructure projects like super-highways, and metros and airports even if it’s a 20 year return on investment. But investing in health care for children, which would also be a 20 year return, just doesn’t make sense to this type of economics. Such public expenditure is perceived as less beneficial, unless in some way, it can also be leveraged to provide a stimulus to further private corporate profits. This is part of the attraction in policy makers for shifting to purchasing care and would explain how such purchasing care plays out. If we remember that a considerable part of GDP growth and rise of corporate power in India today is consequent on public expenditure, we would be less surprised by this being repeated in the health sector.
Changing this situation requires a political call. But so much of this level of politics happens at the level of the bureaucracy. Their ideological framework influenced by an uncritical consumption of the global economic discourse and technical assistance from corporate consultancies, could be the bigger barrier as compared to even the elected politician. Public health professionals need to be able to address many such issues if they are to be successful in making the case for expanding public health expenditure.
SS: So we have covered quite a significant bit of perspectives on how to regulate the private sector, the design flaws which exist in private sector engagement and PPPs. But what do you think are the design flaws within the public sector? And I mean, other than inadequate financing and the political will to invest in the public system.
TS: One flaw, that the WHO itself has highlighted, especially in the South-East Asian region, is the need to make primary health care the foundation of UHC. Though this is now acknowledged by many, there is a serious problem in the understanding of primary healthcare approach and it is most often confused with primary level care which only deals with the front line or first contact care. The conceptual understanding of a primary healthcare approach consists of deploying a team of front-line health care providers who not only provide comprehensive family level healthcare support to every individual and family registered with them, but are also able to act as guides and counsellors to facilitate access to higher levels of care thereby ensuring the continuity of care for each individual with healthcare needs. Building the primary health care approach envisages all the facilities of the entire district health system and a good part of tertiary care system as well. Most primary level care, except perhaps a few skin diseases, implicitly requires adequate secondary and tertiary backup. So if frontline workers may be providing antenatal care for all pregnant women, but unless a woman with eclampsia or severe anaemia has got a tertiary care facility available to address this problem when it is detected, it doesn’t make much sense to do primary care. Similarly primary health care is the best for primary and secondary prevention in rheumatic health disease, but without health valve surgery as required, this is not complete. Or for example screening for diabetes and attending to diabetic retinopathy. So development of integrated two way referral systems is an important element of the primary healthcare approach. Other than this the primary healthcare approach requires community engagement, it requires social participation, it requires close the community delivery of care and it requires the greater emphasis on prevention and promotion as compared to curative care- all of which are difficult to build into purchasing contracts. So necessarily all primary health care approach requires a network of public providers and facilities that are providing free care. There are special services and special areas where supplementation from private sector would help, and those who want to contribute must be encouraged- but the main architecture has to be by public providers.
The other big problem is the losing battle against the integration of vertical programmes. Part of the problem is conceptual- the inability to visualize how care occurs through the mediation of the primary care provider and how continuity of care across levels is established. But part of it is also this notion of addressing each disease by a separate technical package, validated by cost-effectiveness studies, that is added on the minimum package of services. This fragments care, creating duplication in supervision, monitoring, supply chains and technical support that extends all the way from the district to the global divisions of WHO Geneva. So therefore, even in the recent assembly, secondary and tertiary care is discussed in one resolution, organ transplantation in another, and primary care in yet another and these are not sufficiently linked or cross-referenced. But another problem is the huge pressure coming on prioritizing certain vertical programs. A good example is what is happening with tuberculosis. While the main problem is that due to marginalization many patients have not even been identified, the required expenditure to manage those who have not been identified is insufficient due to the demand for higher technologies and more demands on workforce time. Some other new verticals and immunizations that are coming in could be even more skewed, like a recent proposal for population screening for fatty liver. There is great keenness on screening in so many forms, but screening is viable and ethical only if you are able to provide care for those who are screened and found to be positive. That lags far behind.
In such fragmentation, public systems are persuaded into introducing vertical programs as a whole lot of activity load on the frontline workers which consumes their time and their effort without providing a corresponding health outcome and which takes time away from comprehensive care responsive to local needs. One example, frontline workers in one state spent an entire month on making lists of all people who are in a risk category so that they can be given BCG vaccination against tuberculosis. BCG vaccination against adult TB has weak evidence to support it. It makes even less sense to deploy so many resources in making lists of people who should get this vaccine, when it becomes available. But this vertical intervention draws away that time which they should have spent on responding to the healthcare needs of each family. And this is only one vertical within the TB programme. Others are active screening, preventive treatment for TB, and so on. Often front-line workers are burdened with non-health outcome related administrative tasks as well. And then there is the huge amount of load of work on digital entry.
So on one hand governments are unwilling to invest in an adequately sized team for primary health care and on the other whatever time the available team has is frittered away into activities with very low health outcomes, creating immense frustration amongst health workers.
In short, there are serious flaws in the organization of work at the front line. The WHO’s silence does not help. Because policy makers are quick to conclude that “look, we have invested crores in public provision of primary care but it did not deliver and therefore we need to privatize.” But privatization or purchase from private sector does not address these issues either. The family visits of frontline workers should advise people according to risk at all age groups, instead of address one targeted disease and that too by filling a form or data entry. When it was only a small set of priorities it worked, but as more interventions get added on, it becomes impossible to increase the burden of work on the frontline worker. It has reached natural limits. And therefore, service coverage has halted at the selective indicators And, we are also selecting indicators limited to what they are able to do rather than capture what needs to be done. This should help us understand why primary care networks of most LMICs after two decades of selective health coverage are now unable to improve service coverage further.
Yet another issue is with regard to universalising access to essential technologies. It has to be affordable to healthcare systems. This requires that the terms of innovation, the intellectual property regimes, manufacture and supply chain management and quality assurance or all such that it is affordable for public procurement. Countries like Thailand, Bangladesh and Sri Lanka have most essential drugs manufactured and procured by public pharmaceuticals can ensure greater progress at a lessor budgetary expenditure.
Another major constraint is the lack of a legal framework to drive government intervention. Our contention is that we are not going to achieve “universal health coverage” or “Health for All’ in the developing world without a rights-based approach that is reflected in the country’s’ legal framework. A legal framework is required to guarantee public health standards in proximate social and environment determinants like drinking water, sanitation, pollution control, occupational health etc, with respective government sectors accountable to addressing them. But in health care also, in a context where we are not depending on market forces to close the gaps, we need a legal framework to ensure that government provides the health services that can ensure universal access to healthcare without financial hardship- in other words a legal framework for UHC. Such a law, in line with the UKs NHS Act or Thailand’s National Health Security Act should in the least specify key features of the health services that are required. These features would be that every resident is entitled to a primary care provider, and that such a network of providers provides the care required or provides the access to all the care that is required. Where a specific provider or facility is not able to provide the care required it becomes the obligation of to ensure a facilitated referral to the nearest and most appropriate facility that can provide that care. Then and only then, would we be able to ensure a primary health care approach. Without this right, you allow the patient to seek care for themselves, including in the market place. The earlier understanding was to limit public services to a minimalist selective package and leave the rest to the private sector. This did not work, and it led to poor service coverage, increasing healthcare-foregone, and huge out of pocket expenditures. And this is what is perhaps reflected in the UN and WHO documents that we began this conversation with. If we are indeed serious about universal healthcare, then such a legal framework becomes essential. This approach also helps uncover latent disease. There is a huge burden of undetected, untreated diseases or inappropriately treated diseases that will now be able to access quality care. The right to healthcare is very much part of the WHO mandate and in one set of UHC indicators this even appears as an indicator. But this too is missing from all the reports and resolutions of the recent years.
These design issues go along with the two core implementation issues- adequate funds to support the required service delivery and adequate human resources. Of these the one area where finance ministries are most reluctant is to provide the sanction for hiring and deploying adequately staffed well trained primary care teams and ensure that public hospitals are adequately staffed.
SS: But do you see any role for the private sector?
TS: Given the huge demand for healthcare the private sector would have a role. But the government role would be largely regulatory- in ensuring ethical practices, quality of care and reasonable rates. We know that due to information asymmetry this cannot be left to private care providers. But there is also an important role that they can play in supplementing public health capacity. A modest number of hospitals either because they are not-for-profits or because they have under-utilized capacity would be ready to participate at reimbursement of marginal costs. In addition a number of empanelled hospitals could be contracted to receive referrals from the public sector because when the public sector capacity has been exceeded. For example if in the public sector, my waiting list for a coronary bypass surgery has exceeded 2 months, these would be referred to contracted private sector units. And such hospitals would be duty-bound to provide that care, free of cost and within agreed upon time standards, and government would be obliged to reimburse them the costs of care. This is not a new proposal. This is exactly what the National Health Policy articulates. All we are saying is: please take your policy seriously.
SS: We started off from the point that progress to UHC is off track. But do we have reliable measures of progress? What are some of the challenges which are faced in measuring the progress towards UHC?
TS: One priority is reliable mortality data for measuring outcomes. Preferably aggregated at district level in real time. Is this a reasonable and feasible demand? Note that in India, and in most LMICs fairly extensive and robust civil registration systems already exist. In many states on India they capture over 90 percent of mortality and further the data is already available in a computerized format. What we really need is to generate indicators and use this data and this will in parallel improve validation and quality of data. Just like under 5 mortality rate earlier, preventable mortality in the 30 to 70 age group, disaggregated by gender and age, is a key indicator of health outcomes of UHC. Of course, the traditional value of maternal mortality rates and under-5 child mortality rates would continue. Mortality rates of 5 to 15 and 15 to 35 would also be valuable. Detailed cause of death is not essential at this stage and broad symptomatic categories would be enough. International reports often use global burden of disease estimates generated by IHME. That is a poor substitute for mortality based measures and better avoided. (to be discussed further in a subsequent conversation).
The second priority, would be to measure unmet healthcare need for key services using sample household surveys. This would capture prevalence of latent illness and care forgone. In one study in a tribal district, only 1 in 2 diabetics, 1 in 4 hypertensives were picked up. (Ranjan et al, 2023) The rest was latent. In arthritis only one in two wer epicked up but inappropriate care characterised most. In clinically significant depression, only 5 in 100 cases had been identified and put on appropriate care. This high degree of latent disease is related to the both awareness and access. If coverage is measured by utilization figures alone, one may get high levels of utilization, and yet you may have high unmet needs and both could rise in parallel. For examples even in districts or states where C-section rates are over 50, but unmet needs for caesarean section also remain high. Similarly diabetic care utilization goes up but unmet needs for diabetic retinopathy care are also increasing. The inclusion of unmet needs is something that the WHO is seized of thanks to a resolution moved by Thailand and a number of countries with Prof. Viroj in the lead. But there is as yet no roll out.
And a third priority is periodic measures of financial protection on the model of NSSO 71st and 75th round sample household surveys. Unmet needs, Utilization of care and costs of care can be measured in the same survey. Currently we only have the National Family Health Survey (also known as the demographic and health survey in many countries).. This is a good survey but focussed on maternal and child care and already overloaded. These UHC measurements of coverage and financial protection require their own survey, but institutionalized and quality assured like the NFHS. A survey once in 3 to 5 years should be adequate.
In summary, if any country is serious about measuring progress towards universal health care then it needs to strengthen its mortality reporting systems, it needs to measure unmet need and it needs to have periodic measures of out of pocket expenditure and catastrophic health expenditure done in a systematic way. The latter two measurements could require a well-designed household sample survey. All these data should be suitably anonymized and available in the public domain with disaggregation by sex, economic quintile, social group and geography. This is going to be very important in the progress towards UHC.
SS: Yes. Disaggregated data becomes very important. That’s another challenge that we see in current indicators and framework of measurement – they are measuring coverage but equity remains a question mark.
TS: Reliable equity measurements tend to come from well designed community-based sample surveys. The HMIS system is not a reliable or feasible source as of now. This needs to addressed separately, on another occasion.
SS: Another question that I had was about actual coverage versus effective coverage. So if you see the current service indicators, there’s not much to say or even reflect on whether quality of care is indicated within these services. So do you have any thoughts on that?
TS: We are largely looking at quality in terms in terms of clinical effectiveness. Quality in terms of acceptability, dignity, comfort and convenience is to some extent reflected in unmet needs. That’s a proxy indicator but it’s not a very reliable for quality. Unmet needs have many more causes.
Even for clinical effectiveness of care, at this point of time, the best that our current sources of data could tell us is whether care is provided by a certified facility or qualified provider. We can limit the measure of utilization of care to formal care providers and exclude care provided by informal providers. We know that MBBS providers do not necessarily mean clinical effectiveness. But that is where we are. If our objective is progress towards UHC, then the objective is how many get care from a qualified provider and later we could include from quality certified facilities. That would make sense since other than training to providers and quality certification through NQAS we do not have any other intervention for addressing quality of care issues.
SS: We are almost reaching towards the end of the interview. But before we close, do you have any thoughts on the role of global civil society in this debate about the inability to meet the UHC targets. We have so many different forums like UHC2030 and Joint Learning Networks etc. What role have they played in moving or pushing the agenda with UHC, particularly in the interest of low- and middle-income countries?
TS: It is difficult to comment. There is a diversity of organizations with different priorities. A sizable section of civil society itself is dependent upon international corporate funding. Civil society positions could range from actively supporting or facilitating different forms of market-based care to rights-based organizations which strongly oppose privatization. Some organizations act as agencies manufacturing consent for corporate providers and promoting the dominant discourse, others see a career opportunity in implementing the dominant policy without raising critical questions about it. But there are many organizations who are able to pose alternatives and foster a critical dialogue about strategy. Overall, despite these differences they have helped raise issues related to lack of investment, equity allocations, and lack of workforce policies. And therefore overall they have made a positive contribution. However, when it comes to the way forward, it is better to conceptualize civil society forums as a terrain or platform to foster a better understanding of why UHC is off track and a dialogue on the corrective actions required, rather than to project them as saviours and governments as failures.
SS: So the last question I have is about whether UHC was a wrong slogan or is it already a wasted opportunity? Or has it helped and led to positive changes?
TS: Universal Health Coverage has happened- as a discourse, as a way of thinking and talking about universalizing healthcare or health for all as a desirable goal for all of society and all of governments. The notion that all healthcare could and should be free, surprises, even shocks our administrators, senior professionals, elite. For them to know that such an objective has international acceptance is a big step forward. Because in the earlier “structural adjustment” discourse, government was limited to a very selective interventions and left the rest of the markets. Now there is a serious debate over the roadmap, which this conversation discusses. But the fact that the goal has been established and accepted, that it is part of the international consensus built into the SDG goals, and that progress towards the goals is measured and reported, and that this lack of progress has been made visible honestly and with integrity – all these are very welcome and hopeful measures in the long struggle for health rights.
SS: I just wanted to ask one last question before we wrap up. We are already halfway into the 2030 agenda and still deliberating design flaws and needs for course correction. Do you think such kind of dialogues are happening particularly in India at the state government level? Is anybody even reading the UHC2030 report, noting the poor progress and taking some actions?
TS: There are grounds for optimism. In health policy, whether it is tuberculosis or universal health care or economics and health for all, the relationship between policy developments at global level and the country level is very close. Initiative at the global level have their resonance in the country level within the next year or two. This is unlike say, what happens in education sector or agricultural sector. And since these debates are present at the global level, there will be considerable awareness at the country level too. And the interventions of People’s Health Movement’s interventions do resonate across countries. Of course, countries which are more responsive to their populations, more democratic and less autocratic would be more responsive. But it is not enough to acknowledge the problem. There must be actionable alternatives. While some changes require major social and economic transformations, there is much that can be done even within current regimes, and this will strengthen the case for further changes.
Acknowledgements:
Ms Roubitha David for her contribution to recording and transcribing and editing the interview. And Ms Riya Raghunath for her front-page illustrations.
We also gratefully acknowledge that much of the content of these discussions are drawn from the Peoples Health Movements Commentaries on the UHC discussions in the 77th World Health Assembly and United Nations General Assembly sessions as published in the WHO Tracker. The content has been adapted to suit this audience. This is part of the effort to make the global policy developments and debates more accessible to the public health community and civil society organizations at the country level. We take responsibility for any errors or change of meanings that may have been inadvertently made. We also encourage readers to follow the PHM comments on this as they evolve in the WHO tracker


Useful article.
However, I fell regardless of how comprehensive and expansive we make the two UHC target indicators along with unmet health needs etc, survey methods alone may not complete the picture to give a sense of equity, and quality issues. They hide more than reveal the progress of UHC especially when implemented as PHFIs. We should demand/emphasize on more good context-based (country/state) qualitative studies and policy analysis to understand the equity concerns.
It is also interesting how in the media sometimes, the focus ends up being more on the financial protection indicator with the government /even technically strong NHA people rushing to publicise it without complementing it with the service coverage indicator (though limited), even when the methodology says that both indicators should be “monitored jointly”.